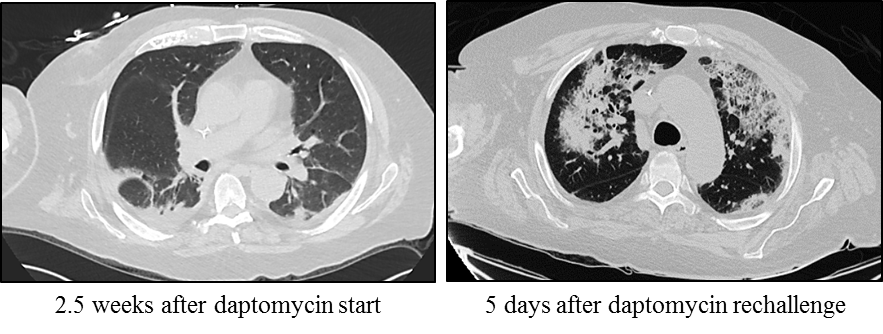
Case Presentation: We present the case of a 70-year-old man who developed MSSA bacteremia after removal of a spinal stimulator. The bacteremia cleared with cefazolin treatment, but he developed an MSSA psoas abscess. He underwent abscess source reduction and was started on oxacillin, based on culture sensitivities. Unfortunately, he developed encephalopathy and was restarted on 6 weeks of cefazolin. At follow up to his PCP and Infectious Disease specialist, he had new shoulder pain and an elevated ESR. His antibiotic duration was extended to a total of 8 week and imaging was ordered to explore the cause of his pain, which did not improve despite completion of antibiotics. He was readmitted for sepsis, shoulder periprosthesis infection, and blood cultures re-demonstrating MSSA bacteremia. He received surgical shoulder washout and was started on vancomycin, due to failure of cefazolin treatment, but then developed an AKI. Infectious Disease recommended daptomycin and he was discharged to complete home infusion. Four days later, he was readmitted with fever and acute hypoxic respiratory failure. CT showed patchy panlobar ground glass and interstitial opacities. The differential included hospital-acquired pneumonia and daptomycin-induced lung injury, and daptomycin was stopped with symptom resolution in 24 hours. After discussing with ID and the patient, he was rechallenged with daptomycin and remained asymptomatic for 24 hours before discharge. Four days later, he was readmitted for worsening hypoxia and repeat CT showed significant worsening multifocal airspace disease. Given the high clinical suspicion for daptomycin-induced lung injury, he was switched to vancomycin with complete symptom resolution within 24 hours of daptomycin removal. A bronchoalveolar lavage was deferred after discussion with the patient and a pulmonary specialist. Despite close monitoring with serial BMPs and vancomycin levels, he developed an AKI and was switched to linezolid. He successfully completed the antibiotic course without further adverse reactions.
Discussion: This case demonstrates complications from MSSA infection and treatment, including the rare daptomycin-associated lung injury. It also demonstrates the immense value of patient involvement in decision making, even in such a complex clinical scenario. There are 37 reported cases of daptomycin-associated eosinophilic pneumonia. Similar to this case, most affected patients are male, elderly, and present 1-4 weeks after daptomycin initiation. To date, no in vitro studies have demonstrated the pathophysiology of this condition, however it is hypothesized to be related to an interaction between daptomycin and pulmonary surfactant.
Conclusions: This case highlights the importance of considering daptomycin-induced pneumonitis in hypoxic patients who lack other identifiable causes. It also emphasizes the benefit of a multi-disciplinary approach in the diagnosis and management of complex patients, with patients sharing in the decision-making process to improve outcomes.