Background: Effectively screening for sepsis in a hospital setting remains an elusive goal. Designed processes have been plagued by poor specificity [3,5], leading to alarm fatigue [2] and overuse of resources. Electronic tools have attempted to automate some or all screening, but thus far to inconsistent success [1]. Furthermore, for patients screened as septic, quickly enacting the Center for Medicare and Medicaid Service (CMS) SEP-1 bundle of interventions constitutes a major challenge to already strained workflows. Obtaining needed lab work, providing indicated fluids, and saving lives with timely antibiotics requires coordinating multiple disciplines in rapid sequence. Frequent fallouts in this bundle of interventions lead to compromised care and ultimately greater mortality. [4]
Purpose: The goal of this project was to reduce sepsis mortality at Tampa General Hospital (TGH), a 1040 bed comprehensive academic medical center. TGH cares for a high risk and diverse patient population as the area’s only level 1 trauma center as well as housing adult and pediatric burn centers, a transplant center, and a nationally certified stroke center. Prior to this project, a lack of real-time visibility into care provided to septic patients led to delayed diagnosis and frequent fallouts in the CMS SEP-1 bundle.
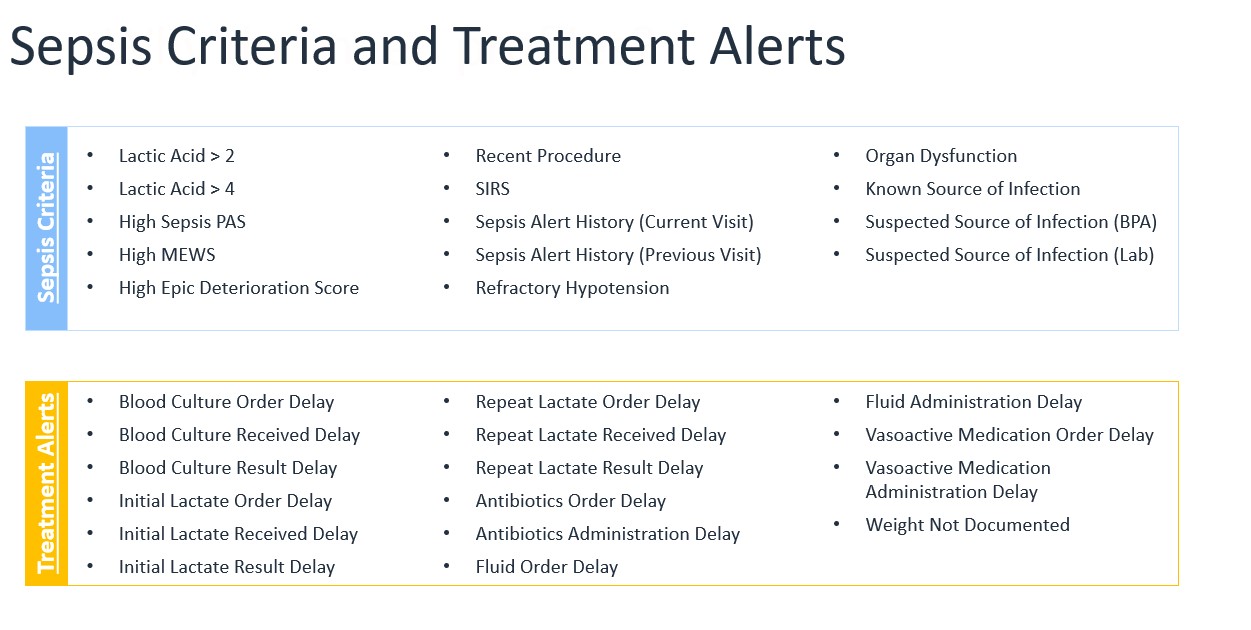
Description: The pilot project combined innovative technology with trained staff to improve sepsis recognition and reduce time to appropriate treatment. In partnership with GE Healthcare Command Center, we developed the TGH CareComm Sepsis tile which is a real-time data interface focused on early detection of patients at risk for sepsis, as well as compliance management in treatment protocols for patients diagnosed with sepsis. The tile gathers real-time EHR data and applies rule-based algorithms to monitor 14 different risk criteria for sepsis (fig. 1). At-risk patients are presented in a prioritized manner for evaluation by a trained Rapid Response Team nurse. This evaluation may include chart review, discussion with the bedside nurse or covering provider, or in-person assessment. Once a patient has been diagnosed with sepsis and is in the treatment pathway, they are monitored to ensure that appropriate treatments, including antibiotics and fluids, are ordered and administered in a timely manner. Flags for treatment delays appear at predetermined timepoints, allowing the Rapid Response Team to interface with frontline clinical staff and address barriers to high quality care. For example, a patient who has an order for antibiotics but has not yet received them after 1 hour will trigger a flag, and the RRT Nurse can communicate to the bedside to troubleshoot the delay.
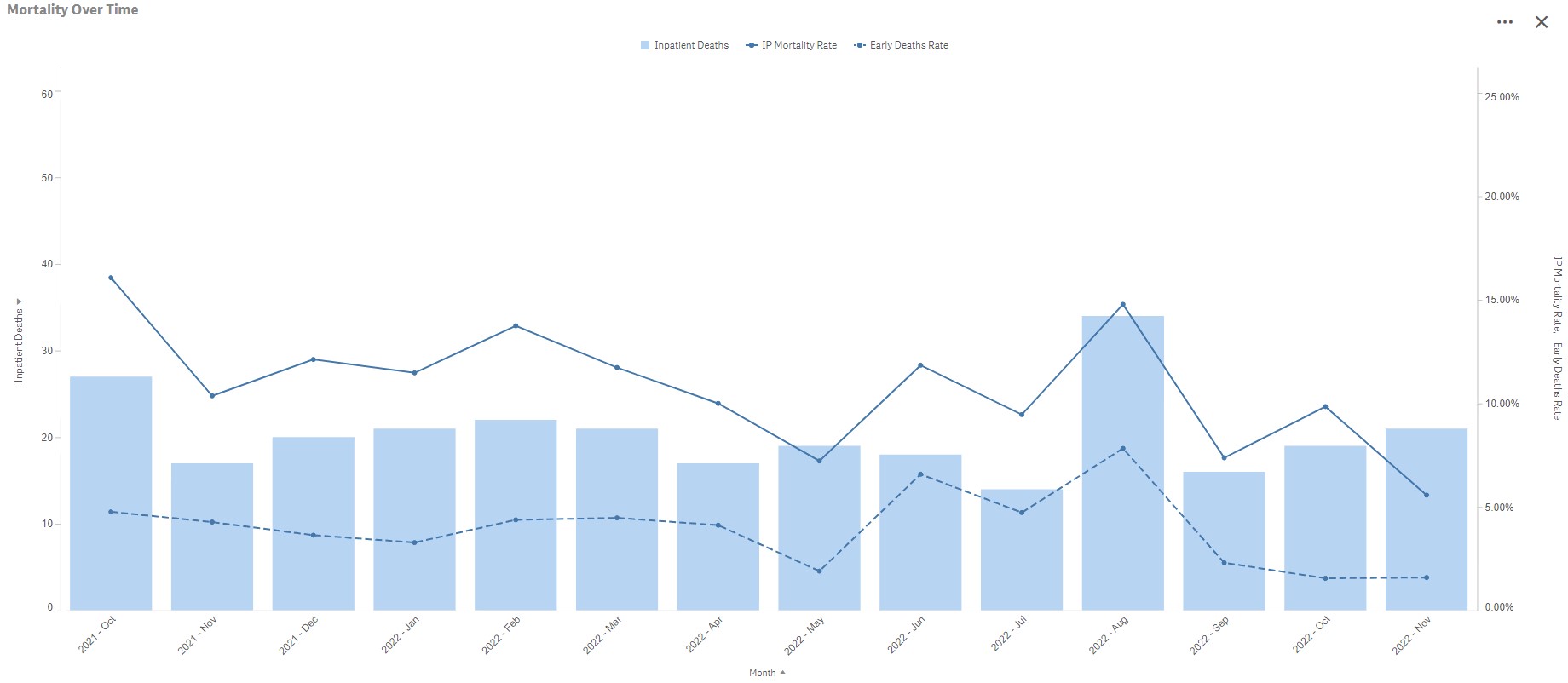
Conclusions: In the 3 months since initiation of this project (8/2022 to 10/2022), our average sepsis mortality rate for DRGs 870-872 has been 6.19%. This compares favorably to the Fiscal Year 2019-2021 average mortality rate of 9.26%. Our early death rate (rate of mortality within the first 24 hours after presentation) is 1.78% for the same 3-month span, with a previous average of 3.20% (fig. 2). Regular feedback on opportunities and organization-wide support of the effort has led to these early gains. Perhaps more importantly, the added transparency into care systems has allowed for process improvement cycles focused on fallout trends. The triad of people, process, and technology has been key to these effective improvements.