Background: US healthcare costs are exorbitant and excessive lab utilization contributes significantly1. Daily labs (DLs) are often over-ordered for inpatients.2 This leads to increased costs, iatrogenic anemia, patient discomfort and limits phlebotomy resources 3. The Choosing Wisely® campaign recommends against checking DL in patients who have clinical and lab stability5. Previous quality improvement initiatives have improved lab stewardship without increasing length of stay, readmission rates or mortality.
Purpose: Patients discharged to skilled nursing facilities (SNFs) often experience significant delays in discharge as they await non-medical needs which places them at risk of additional days of unnecessary lab draws. Our study aimed to reduce over-ordering of DLs and labs on discharge (LOD) on this population through several interventions delivered on a hospital medicine teaching service.
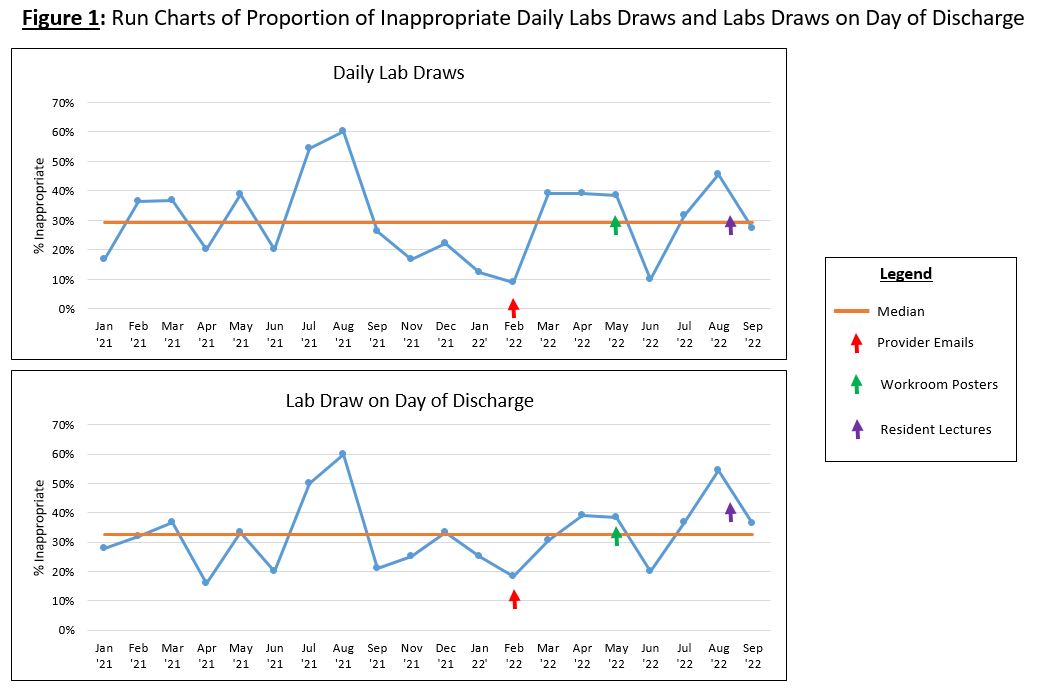
Description: This study was conducted at an urban academic tertiary medical center on 2 services each consisting of an attending hospitalist and third year resident (PGY3). Retrospective review of general medicine and cardiology patient charts from 02/2021 to 06/2021 was performed to establish a baseline. Only patients who were discharged to SNFs were included. 6 hospitalist attendings and one resident served as reviewers and assessed when DL and LOD were present. DL was defined as either a BMP, CBC or both present every day of hospitalization. Physician reviewers assessed the appropriateness of DL by reviewing documentation present and lab values. Lab appropriateness guidelines were agreed upon by reviewers to reduce subjectivity. Several educational interventions were then enacted (table 1). First, emails were sent to hospitalists prior to their rotation asking them to focus on teaching their PGY3s lab stewardship. Next, posters were placed in workrooms reminding providers to avoid ordering DL for patients who were only awaiting SNF placement. Lastly, a lecture was delivered to the PGY3s about lab stewardship. This was followed by a sample patient chart review case and dissemination of the lab appropriateness guidelines to the PGY3s. Post-intervention data was assessed by chart review of patients admitted between July 2021 to October 2022 in the same manner as the pre-intervention data. The educational interventions have not reduced the amount of inappropriate lab utilization thus far (figure 1). Future interventions planned will include electronic health record (EHR)-based prompts and feedback to healthcare providers on their lab ordering.
Conclusions: Lab utilization remains an area in need of improvement at our institution. The initial phase of our project, consisting of educational interventions, has not significantly reduced the amount of inappropriate DL or LOD. Further interventions are planned, including EHR-based prompts and feedback to providers.