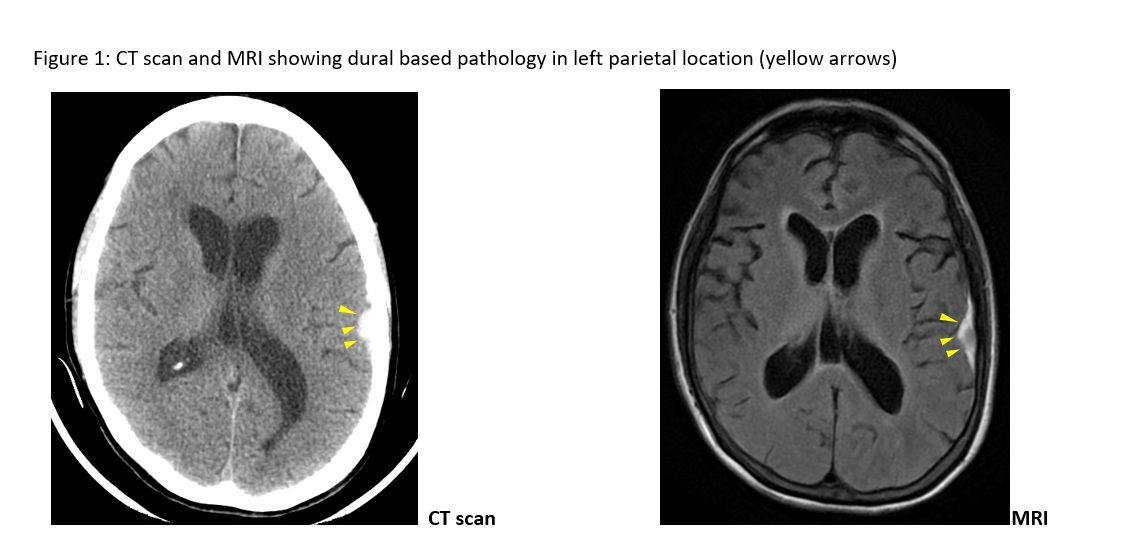
Case Presentation: A 74-year-old female missionary without any past medical history was found unresponsive on the floor and brought to the emergency room. On initial physical exam she was encephalopathic but without any focal neurological deficits and an otherwise normal physical exam. Laboratory results including toxicology were all normal. CT scan of the head showed an acute parietal subdural hematoma without any mass effect. Over the next two weeks, the patient remained encephalopathic, out of proportion of her hematoma. She also developed fever (maximum temperature 101.5 F) and a left sided facial nerve (Bell’s) palsy. Repeat brain imaging including CT scans and MRI reported stable parietal subdural hematoma with no new pathology. No seizures were seen on EEG. CSF analysis showed 200 cells/µL, with 99% lymphocytes, 38 mg/dL glucose (low) and 318 mg/dL protein (high). Blood and CSF were tested for meningitis, Lyme disease, syphilis, prion disease, paraneoplastic encephalitis, autoimmune & anti-NMDA-receptor encephalitis, sarcoidosis, mycoses, tuberculosis and HIV – all of which came back negative. Flow-cytometry of CSF cells showed B-cell lymphoma cells (CD 19+, CD20+, CD5-, CD10-) indicating B-cell non-Hodgkin’s lymphoma. PET-CT scan did not show any other site of lymphoma involvement. The patient died shortly after.
Discussion: This is an interesting case of primary central nervous system (CNS) lymphoma, which is relevant to hospitalists on two accounts. First, clinicians will be well-served to know that there are pathologies like lymphoma than can mimic subdural hematoma. Treatment delays can occur if differential diagnoses are not considered after subdural hematoma is reported on CT and MRI.
The second lesson is the role of cognitive bias and heuristics. This patient’s clinical history was framed as being found on the floor with initial CT scan showing a subdural hematoma. In the next four weeks, four more scans (CT & MRI) were also read as subdural hematoma. Clinical evaluations by several physicians for encephalopathy with non-infectious fever (a B symptom of lymphoma) and left facial nerve palsy failed to recognize both these clues of malignancy, probably due to anchoring bias. Representativeness Heuristic is a cognitive bias that also played a role. Subconsciously, clinicians can make a diagnosis based on how closely a clinical scenario resembles a pre-formed prototypical diagnosis. Instead of considering all the clinical information only certain facts are used to fit the diagnoses that is already made (subdural hematoma in this case). This emphasizes the need for clinicians to be aware of cognitive biases to avoid the pitfalls highlighted in our case.
Conclusions: Cognitive biases like anchoring bias and representativeness heuristic can lead to delays in diagnosis and treatment. Even in relatively straight-forward diagnoses like subdural hematoma, hospitalists should always consider differential diagnoses like CNS lymphoma.