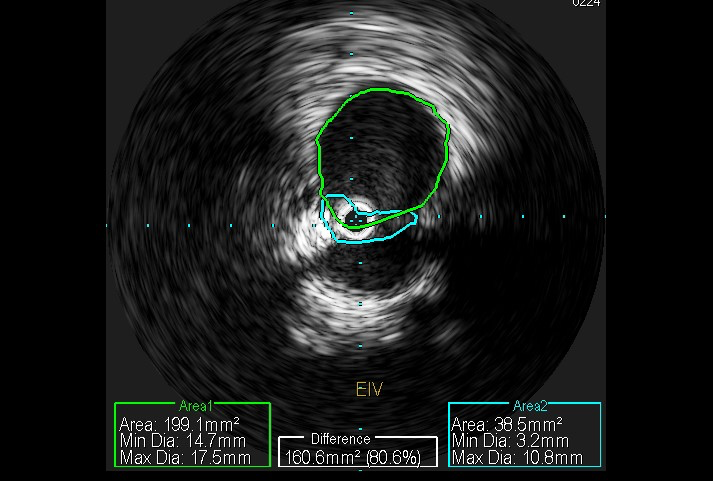
Case Presentation: 73-year-old male with past medical history of seizure disorder, non insulin dependent diabetes mellitus, hyperlipidemia presents for evaluation of pain and swelling of right lower extremity, found to have deep venous thrombosis involving multiple veins of right lower extremity, occlusive in nature. Past medical history significant for two similar episodes of VTE (venous thromboembolism) in lower extremities. Patient had hypercoagulability work up and age appropriate screening for malignancy during initial presentation which were both negative. He was prescribed anticoagulation with different agents each time in past. During this hospital course IVCS (iliac vein compression syndrome) was suspected, Venography with IVUS (intravascular ultrasound) done, bilateral iliac vein compression, right more than left was found, right external iliac vein stent was placed. 90 day follow up showed patient in his usual state of health with no other complaints.
Discussion: VTE is one of the leading causes of morbidity and mortality. May-Thurner syndrome is very popular among clinicians where the anatomical variant is left iliac vein compression by right iliac artery. There are many anatomical variants of it, that occur by birth or can develop in adulthood due to atherosclerotic disease, degenerative diseases of lumbar vertebrae, compression due to foreign material, malignancy with atypical presentations. All these variants should be considered a spectrum of IVCS (iliac vein compression syndrome). IVCS is an under recognized and independent risk factor for development of VTE and just anticoagulation might not suffice and may not give us a favorable outcome(1,2). Since different specialties including cardiology, vascular surgery, interventional radiology, hematology, oncology could be involved in development of care plan, the onus is on us as hospitalists to consider it as a differential diagnosis during inpatient care. CT venography, MRV (magnetic resonance venography) are some of the imaging modalities useful to diagnose this condition. Conventional Venography, IVUS would be definitive in estimating the disease burden. Treatment with CDT (catheter directed thrombolysis) for IVCS with acute VTE achieves good patency and vein function after 5 years of follow-up(3). Endovascular treatment for IVCS provides effective long term patency in patient with or without vein stenting(4).
Conclusions: High index of suspicion is recommended to determine if IVCS is one of contributing factors in cases of VTE. Broadening our perspective regarding suspected patient population would result in higher incidence of diagnosis. Ease of diagnosis with imaging modalities and effective, universally available treatment options should encourage us in taking this extra step for improving outcomes in our patients.