Background: Communication failure during patient handoffs is a common cause of harmful medical errors. Therefore, the Joint Commission recommends that healthcare facilities standardize communication during this process. Intrahospital patient transport represents an instance in which it is crucial to have a standardized handoff approach – as patients are monitored less closely, may experience interruptions in treatment for their illness, and the receiving unit is less familiar with the patient’s clinical background.
Purpose: At our quaternary, academic center, a Medicine Step Down Unit experienced two serious adverse events related to intrahospital transport. To address these concerns, a multi-modal quality improvement (QI) initiative was undertaken. A universal protocol was adopted requiring clinical personnel to accompany patients during transport, as well as criteria for nurses, front-line providers, and respiratory therapists to ensure appropriate staffing. Additionally, the use of a “Ticket-to-Ride,” a written assessment and hand-off tool, was implemented to promote safe patient transports.
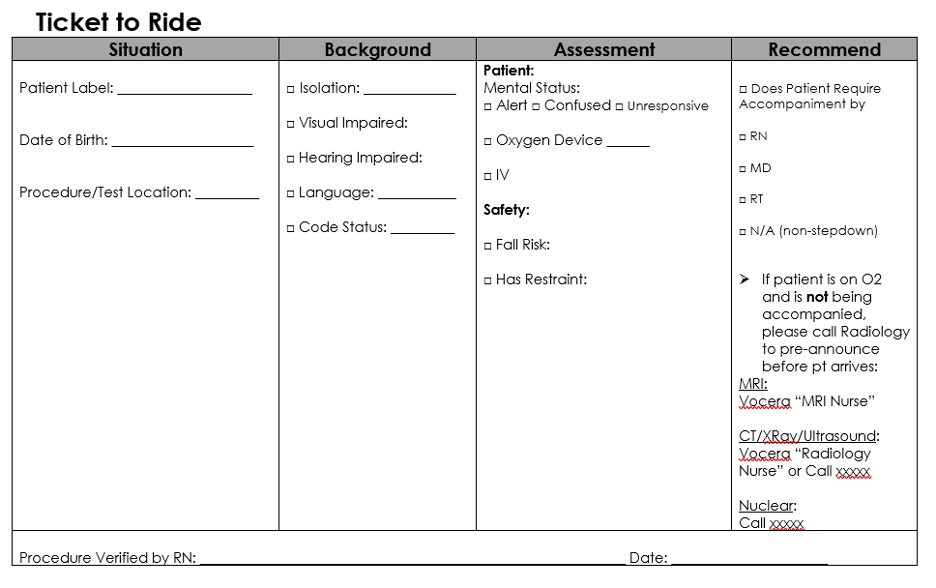
Description: Patient transport tickets were designed by unit staff, including nursing and physician leadership. Input was also gathered from Radiology staff, as most transports were for radiologic studies. A handoff format based on the Situation Background Assessment Recommendation (SBAR) framework was adopted. Patient demographics and procedure location were included in S, characteristics such as language and code status were listed in B, safety considerations were recorded in A, and personnel accompaniment requirements were listed in R. Nurses completed the tickets, which were placed in physical charts that accompanied patients during transport. Upon return to the unit, tickets were removed from the charts and stored securely. Our project consisted of 1) training staff on how to complete the tickets, 2) measuring rates of ticket completion for patients requiring transport on the Step Down Unit from December 2023 – September 2024, and 3) recording the number of reportable adverse events that occurred during patient transport on this unit over this time span. Data from the transport department showed that 1146 transport events occurred during our intervention period. 457 patient tickets were completed (39.9%). There was significant month-to-month variability of completion rates, ranging from 27.5%-55.5%. Safety data, based on review of safety reports, demonstrated that no adverse events occurred during patient transport during the period of interest.
Conclusions: Standardized patient handoffs are critical to patient safety during transport. Close patient monitoring through delineating requirements for patient accompaniment with clinical personnel eliminated safety events during transport. While a Ticket-To-Ride process did not achieve optimal completion rates, it helped in reducing events. We postulate low uptake of our intervention is multifactorial, including insufficient training, high workload, communication challenges, and lack of familiarity with the tickets amongst staff who floated to the unit. Next steps include conducting a post-intervention survey to gather feedback from staff and identify barriers to more successful implementation. By addressing these challenges and improving completion rates, we aim to enhance this intervention’s effectiveness and make it more adaptable for implementation in other healthcare settings seeking to standardize patient handoffs.