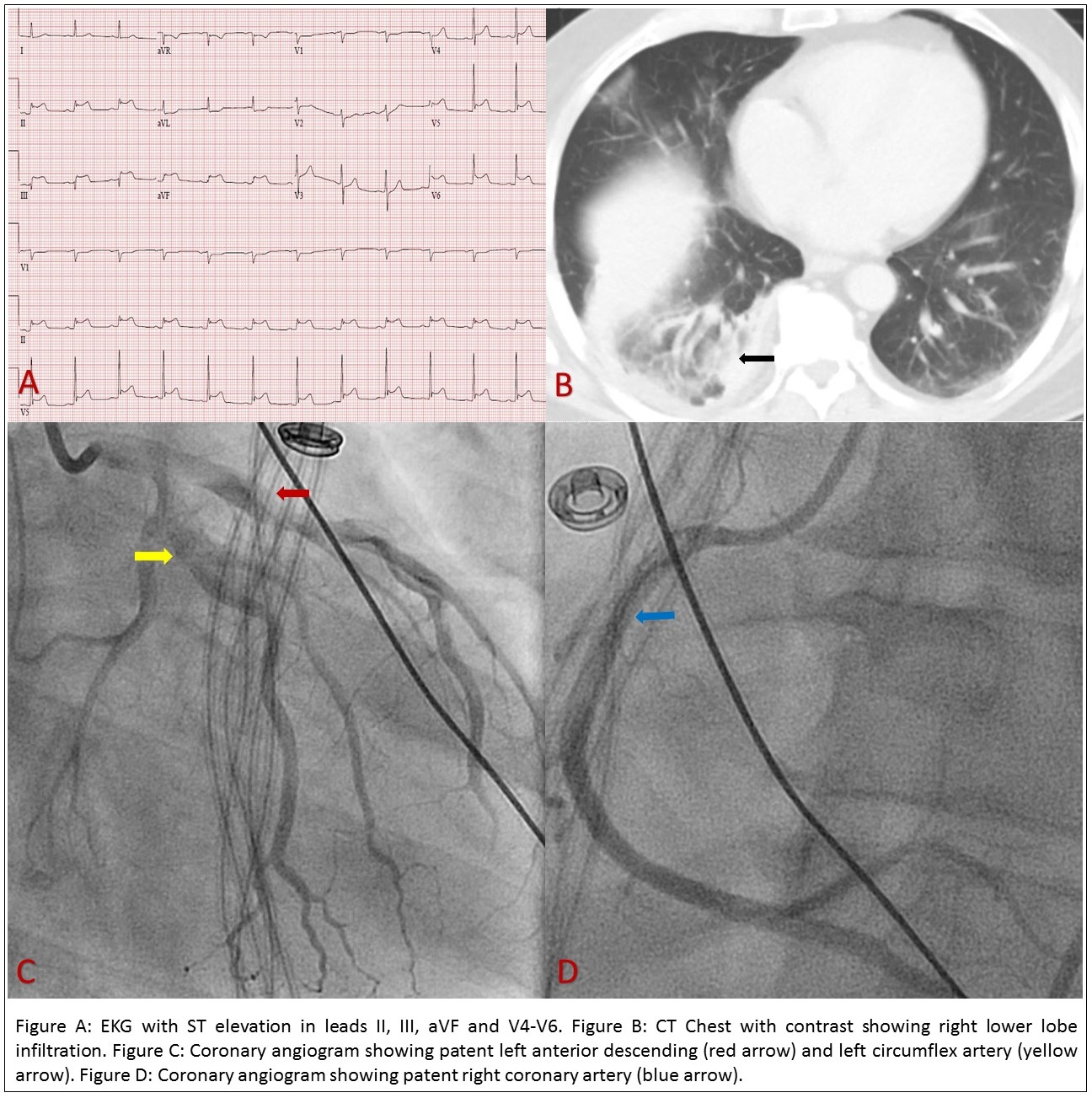
Case Presentation: A 56-year-old male with a past medical history significant for hypertension and hyperlipidemia presented to the emergency department with progressively worsening dry cough, shortness of breath, and non-exertional pleuritic chest pain associated with chills, nausea, vomiting, diarrhea, and generalized bodyache for 2 weeks, worsened over last 24 hours. On evaluation, was found to be hypotensive (BP 76/60 mmHg). Labs showed leukocytosis (17,900/uL, Ref: 4000 – 11,000/uL), creatinine 3.2 mg/dL (Ref: 0.60 – 1.10 mg/dL), lactate 5.8 mmol/L (Ref: 0.5 – 2.2 mmol/L), and troponin 0.65 ng/mL (Ref: <0.03 ng/mL) with no ischemic changes on the electrocardiogram (EKG). Imaging including CT chest showed right lower lobe pneumonia. The patient was resuscitated with aggressive fluids and was started on pressors and antibiotics for septic shock and multiorgan failure. Transthoracic echocardiogram (TTE) demonstrated moderately reduced LVEF 35-40% with hypokinetic inferolateral wall. Heparin was initiated for concern for non-ST elevation myocardial infarction (NSTEMI). During hospitalization, he had worsened chest pain and EKG revealed ST elevation in the inferolateral leads. He underwent urgent left heart catheterization which revealed patent coronaries. Troponin continued to trend up and peaked at 31.78 ng/mL. The patient was continued on antibiotics and eventually discharged in stable conditions, on dual antiplatelet therapy, angiotensin convertase enzyme inhibitor, statin, and beta-blocker. Follow up TTE in 2 weeks revealed an improved EF of 60%.
Discussion: Myocardial infarction with non-obstructive coronary arteries (MINOCA) has a prevalence of 1-12% of all myocardial infarctions. The exact pathophysiology is unknown but possible mechanisms include endothelial dysfunction, microvascular obstruction, spontaneous atherosclerotic plaque rupture, coronary vasospasm, Takotsubo cardiomyopathy, and myocarditis. Sepsis may be associated with elevated troponin and EKG changes including prolonged QTc interval, Osborn waves, nonspecific ST changes, and very rarely ST elevations. (1) In our patient, ST elevation in the inferolateral leads and elevated troponin were likely due to transmural ischemia and myocardial cell damage caused by endotoxins, cytokines, and oxygen radicals induced by the infectious process in the setting of the septic shock. Prognosis of MINOCA patients is generally better than that with obstructive coronary lesions as seen in our patient. (2)
Conclusions: Coronary artery spasm related to myocardial injury following a stressful event (septic shock) is the possible mechanism for our patient with myocardial infarction and normal coronary arteries. It is important to consider different etiologies, other than acute coronary syndrome when approaching patients with acute ST-segment changes and elevated cardiac markers, especially with septic shock.