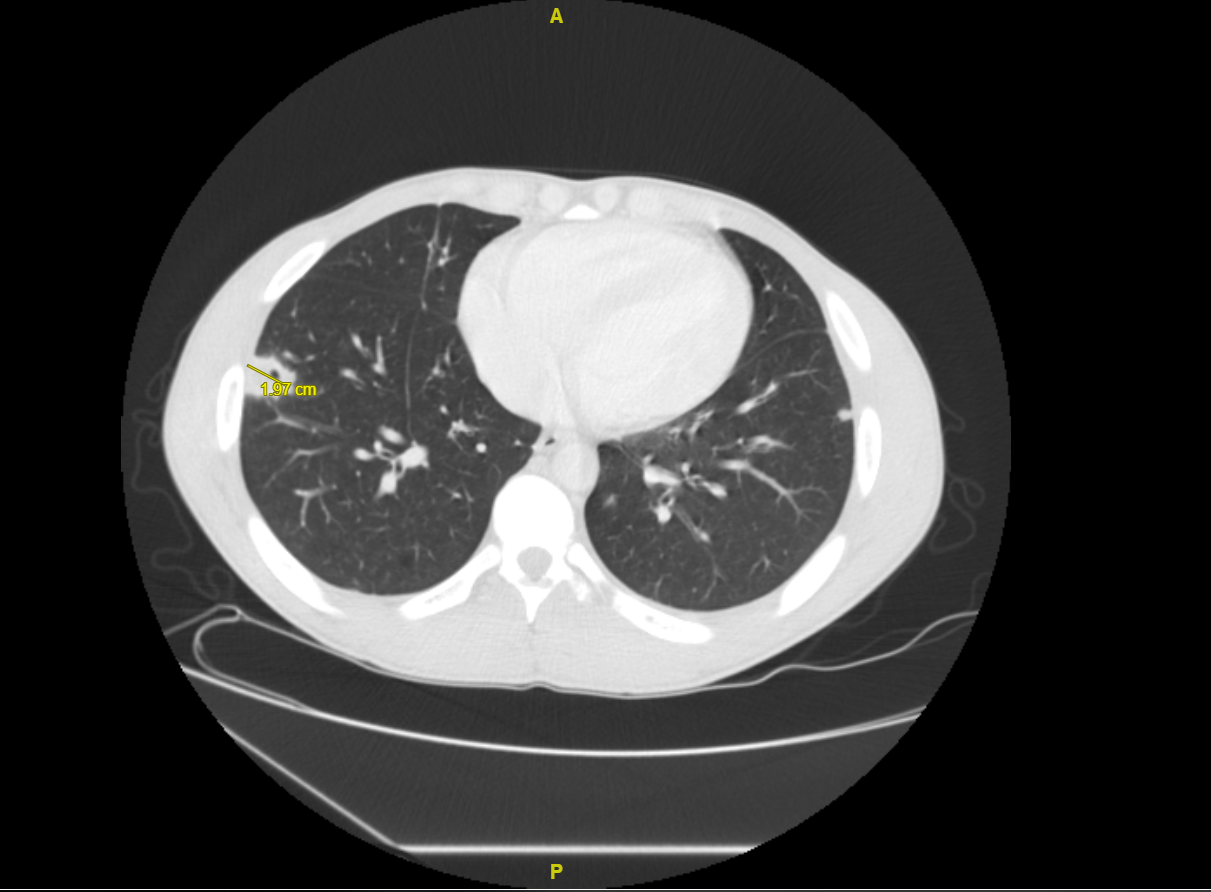
Case Presentation: A 25-year-old man with a past medical history of Ulcerative Colitis (on mesalamine and non-compliant with steroid suppositories) presented as a transfer from an outside hospital (OSH) with fevers, left sided chest soreness, abdominal pain, and bloody diarrhea for 1 week. CT chest, abdomen, pelvis from OSH revealed diffuse colitis as well as several pulmonary nodules. Repeat imaging at our institution, showed multiple necrotic, cavitary pulmonary nodules, initially concerning for septic pulmonary emboli, and the patient was started on empiric antibiotic therapy. The patient denied any history of drug abuse, cardiac history, or dental procedures done in recent past. On physical exam, there were coarse breath sounds, tenderness to palpation in bilateral lower quadrants of the abdomen with no rebound tenderness, and no murmurs, Janeway lesions, Osler nodes, and Roth spots. Laboratory markers were significant for elevated ESR, CRP, and fecal calprotectin. Infectious etiologies were negative for HIV, Hepatitis B, Histoplasmosis, Coccidioidomycosis, Blastomycosis, Coxiella Burnetii, Brucella, Clostridium Difficile, Aspergillus, Lyme Disease. Stool culture, ova and parasite were also negative. Cardiac MRI and transthoracic echocardiogram did not show any valve vegetation, and blood cultures were negative. The only autoimmune marker that was positive was ANA. Further pertinent testing was negative for granulomatosis with polyangiitis, microscopic polyangiitis, and rheumatoid arthritis. After a negative work-up, CT guided lung biopsy was done which revealed fibrosis with mixed inflammatory infiltrate containing macrophages, lymphocytes, scatter neutrophils and plasma cells. Mesalamine was stopped as patient noticed return of abdominal pain with it and few case studies showed pulmonary infiltrates with related 5-aminosalicylic acid derivatives. After poor follow up and not initiating any immunosuppressants, symptoms returned one month later. CT imaging showed persistent necrotic, cavitary pulmonary nodules. The patient was then started on steroids and subsequently bridged to biologic agents.
Discussion: Ulcerative colitis (UC) is a type of Inflammatory Bowel Disease (IBD) that primarily effects the mucosa of colon. Extra-intestinal manifestations in IBD are present in approximately 20-40% of cases. Pulmonary manifestations in IBD are rare and have an unknown incidence. Pulmonary manifestations include interstitial lung disease, bronchiolitis obliterans organizing pneumonia, interstitial pneumonitis, and necrobiotic nodules. On imaging, these nodules are well-defined, and are sometimes cavitated. Histologically, they are sterile aggregates of inflammatory cells with necrosis. Before making this diagnosis, a large differential including malignancy, septic emboli, vasculitis, and other infectious etiologies must be excluded. The literature describing necrobiotic nodules in IBD, and specifically UC is scant, and mainly consists of case reports. One other case report showed necrobiotic nodules in a patient with UC. The patient was treated with a two week course of prednisone and subsequent imaging showed resolution of nodules.
Conclusions: Necrobiotic pulmonary nodules are a rare extra-manifestation of UC. It is important that this diagnosis be considered in UC patients presenting with lung nodules. Management consists of treating the underlying UC. It is critical that a thorough infectious workup be done before initiating immunosuppressant medications.