Background: Both the ACP through its High Value, Cost-Conscious Care Initiative, and the ABIM through its Choosing Wisely campaign, have called on clinicians to engage in efforts to improve the value of the care we provide
Purpose: We sought to develop a curriculum to provide internal medicine residents both a theoretical and a practical exposure to these principles
Description: In July 2014, the VIQ curriculum was introduced for the Internal Medicine residency program at UCSD. During a 2-week “jeopardy” block, available interns and residents participate in directed didactic and hands-on learning. Didactic materials focus on self-directed learning (including a video presentation and review of key articles), supplemented with live lectures that address high value care and basic quality improvement methods. The team then engages in a targeted quality improvement project focusing on efficiency as at least one of the outcomes. The supervising faculty member directs the core project, and the residents are encouraged to propose an additional project of special interest to them.
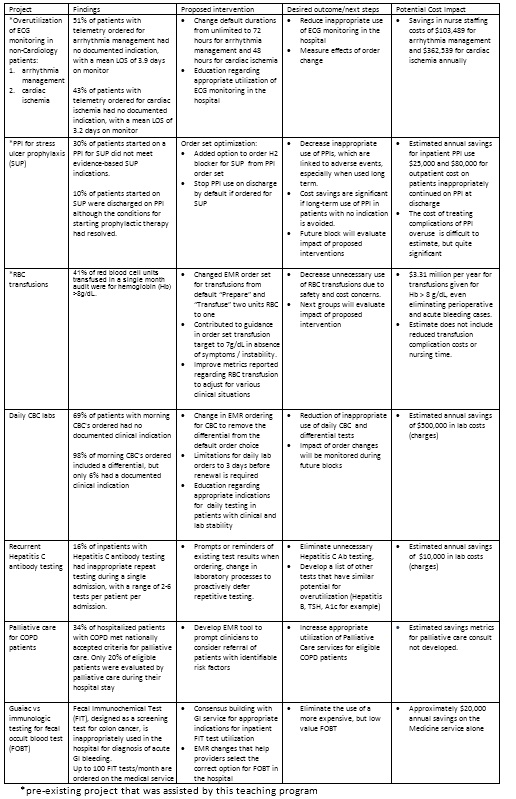
So far, resident teams have furthered efforts on established institutional QI projects during their 2-week blocks, and initiated multiple new projects as well (see Table). A mix of independent teamwork and scheduled meetings with faculty allows a balance of resident autonomy and appropriate guidance. Each group presents a project proposal at the end of the block, which is analyzed for importance of the problem, feasibility, and potential value to the institution.
Because 2 weeks is generally not enough time to develop and implement a complete effort, many projects progress in stepwise fashion, with the work of one team serving as the foundation for work done on future rotations. In this manner we ensure that each group has the chance to complete the steps of a QI project, even if there will be not enough time for them to monitor the implementation.
In the first 5 months of this academic year at least 10 projects were completed. Some have resulted in order set changes in the EMR, others are in various stages of implementation (see Table). Most projects will be followed up during future blocks to track results and fine-tune the interventions.
Conclusions: We estimate that the projects completed during the first 5 months, when fully implemented, can reduce cost of care by at least $4 million annually (Medicare reimbursement rates). In addition, we have introduced the next generation of physicians to a value-driven approach to patient care. Ultimately, we hope to leverage the projected savings to support the faculty and data analyst time required to support the rotation and spread the curriculum to other disciplines.