Background: Patients with substance use disorders (SUD) are frequently cared for by hospitalists and admission presents an opportunity to engage patients in SUD treatment. Currently, patients with SUD are undertreated with medications to treat SUD, despite proven reduction in mortality. Addiction consult services are increasingly seen as an intervention to improve the quality of care for patients with SUD and have shown increases in providing medication for SUD and improvement in patient and healthcare provider satisfaction, however hospital utilization data is mixed, which this study aims to further evaluate. At Northwestern Memorial Hospital (NMH), a large, academic hospital in Chicago, IL, nearly 15% of hospitalized patients in 2023 had an active SUD. Despite this, most patients with SUD did not receive medications to treat SUD. The goals of implementing a multidisciplinary addiction consult service at NMH were to improve patient experience, healthcare utilization, adherence to SUD medication treatment guidelines, and provider knowledge.
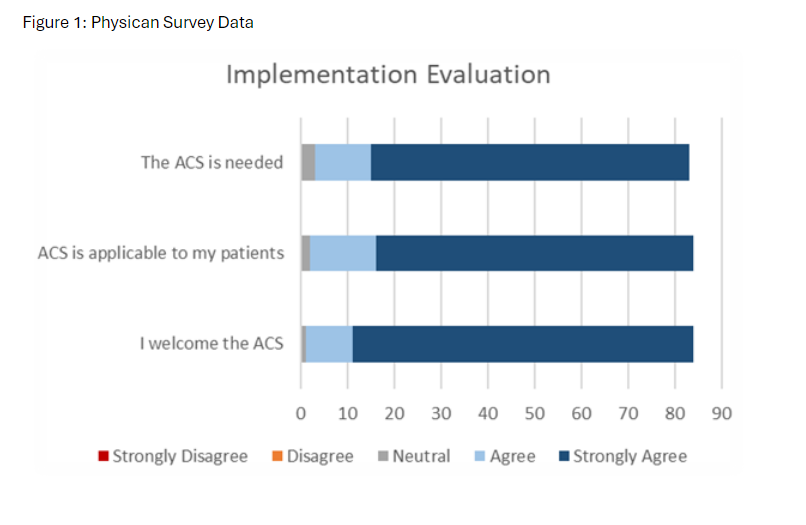
Methods: We developed a multidisciplinary addiction consult service (ACS) with the collaboration between faculty in the divisions of Hospital Medicine and Psychiatry Consult Liaison to meet the needs of our institution. We used the framework of exploration and preparation in years 1 and 2 prior to implementing our pilot service. The addiction consult service launched April 2024 and consists of physicians with expertise in addiction and a dedicated social worker available Monday through Friday during business hours. We assessed patient utilization (length of stay, 30-day readmissions) and usage of medications to treat AUD (MAUD) and OUD (MOUD) during and after admission. We collected both quantitative and qualitative care team (physician/advanced practice provider, nurse, pharmacist, and social worker) and patient survey data to evaluate the implementation process and quality of care. We created elective rotations for medical students and residents across multiple disciplines starting September 2024.
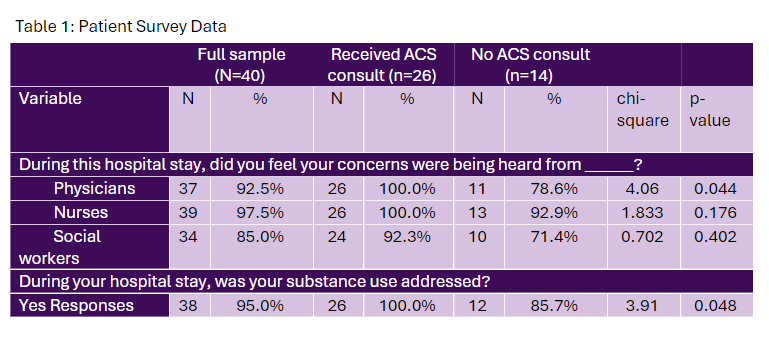
Results: From April 2024 through September 2024, 240 consultations were completed. The mean age of patients was 50 years. The most prevalent substance use disorders were alcohol use disorder (AUD) and opioid use disorder (OUD), respectively. Compared to pre-implementation data, patients who received an ACS consultation were more likely to receive inpatient MAUD (7% vs 59%; OR 18.9 CI [12.8-27.7]) and MOUD (38% vs 98%; OR 150.6 CI [21.0-1082.4]), respectively. Average length of stay (LOS) and observed to expected LOS was reduced by 12% and 23% respectively, compared to historical data (7.52days vs 6.65 days; and O/E 1.01 vs 0.78). Hospital readmissions at 30 days were reduced by 35% (19% vs 13%). Importantly, patients seen by the ACS demonstrated significantly improved satisfaction in feeling their concerns were being heard and their SUD addressed compared to patients with SUD not seen by ACS (Table 1).
Conclusions: Implementation of our Addiction Consult Service was feasible and served to increase MAUD and MOUD compared to historical controls. Patients who had ACS consultation had significantly higher satisfaction in feeling concerns were heard and SUD addressed. In addition, all healthcare utilization metrics demonstrated favorable trends after the launch of an inpatient addiction consult service. These findings support expanding addiction services to improve quality of care and utilization at hospitals with a high prevalence of patients with SUD.