Background:
Academic hospital medicine groups frequently work in clinical care, quality improvement (QI), and medical education, but may not emphasize or have the training to conduct traditional clinical research. However, dissemination of scholarly work is important in academic medicine. We evaluated the effect of a researcher‐led works‐in‐progress (WIP) seminar series on research activities within a division of hospital medicine.
Methods:
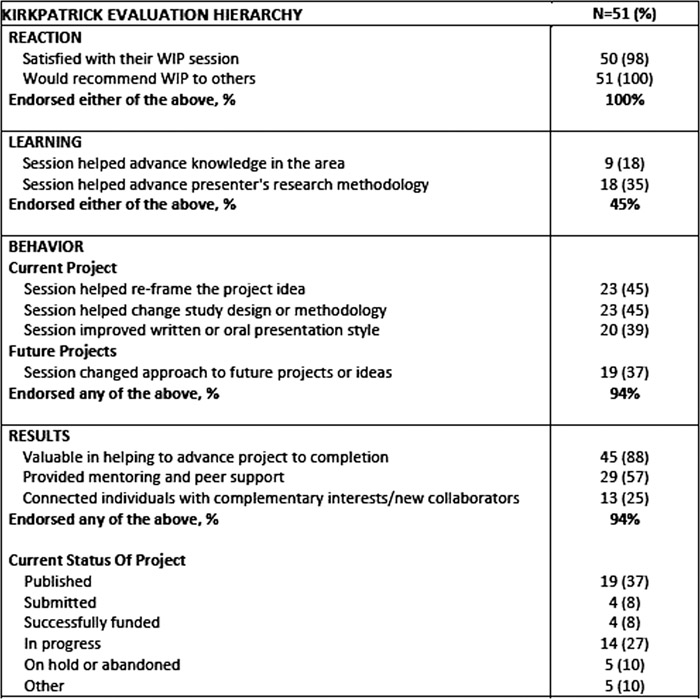
The Division of Hospital Medicine WIP was developed as a weekly forum where members of the hospitalist division could present project ideas or activities in any phase of preparation with the goal of receiving structured feedback from others in the group, including researchers and senior members of the division. We surveyed the lead presenter of 73 WIP sessions from May 2010 to November 2013, and included questions based on Kirkpatrick’s four‐level training hierarchy to evaluate the mechanisms through which WIP helped advance projects to completion: (1) Reaction – participants’ satisfaction; (2) Learning – knowledge acquisition; (3) Behavior – application of skills; and (4) Results of project, including outcomes on scholarly work. We also compared responses for projects led by career‐researchers (defined as hospitalists with fellowship research training and ≥ 70% dedicated time for research) to non‐researchers using chi‐squared tests.
Results:
Of the 51 surveys completed (response rate 70%), 35 (69%) projects were led by non‐researchers. Project topics were diverse, and included QI, clinical research, global health, medical education, high‐value care, and evaluation of health technology. Reaction, Behavior change and Results were all positive with >90% respondents reporting at least one positive outcome in each category and a high rate of publication/funding (Table). Fewer (N=23, 45%) reported a positive impact on Learning/knowledge acquisition. In 49% of surveyed projects led by non‐researchers, WIP led to a change in their approach to future projects, compared to 13% of projects led by researchers (P=0.01), and the WIP led to positive mentorship and peer support for 69% of projects of non‐researchers to 31% of researcher‐led projects (P=0.01). No other significant differences between researchers and non‐researcher projects were identified.
Conclusions:
Presenters at an academic hospital medicine WIP series reported high satisfaction and attributed enhancement of scholarly work primarily to behavior change and results. Non‐research clinicians may benefit more from the mentorship and clinical research training aspects of this WIP than researchers. This study suggests a WIP can successfully promote scholarship for clinicians with a broad range of interests in an academic hospital medicine group.