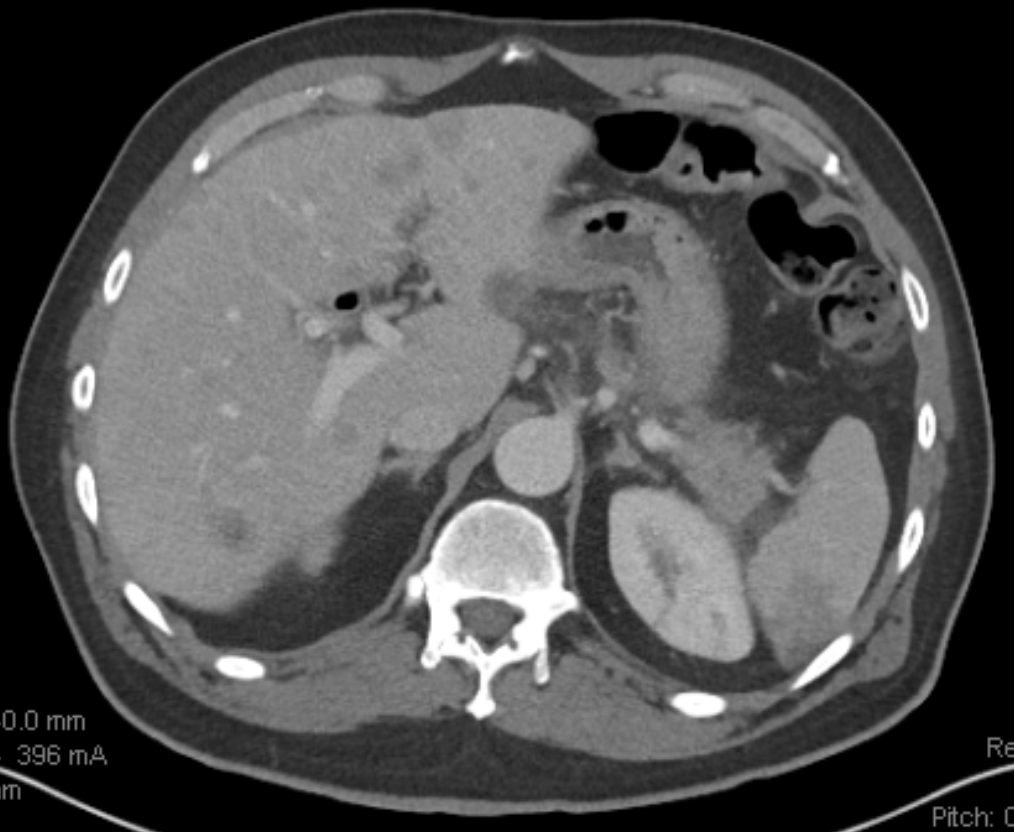
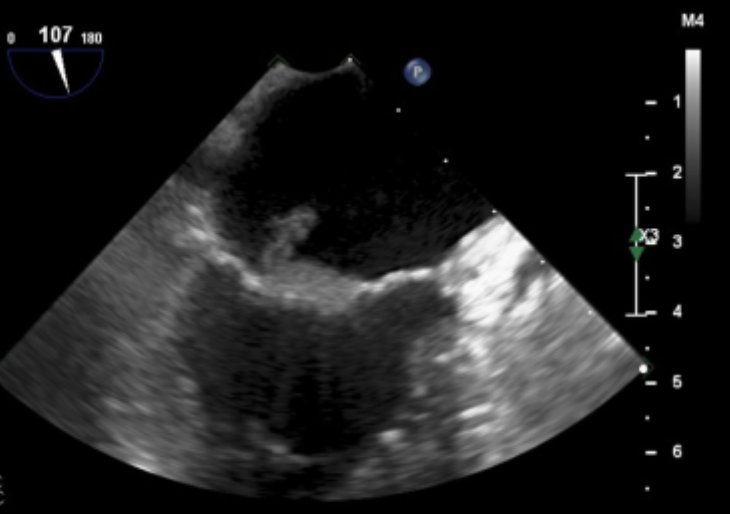
Case Presentation: A 49-year-old man with metastatic pancreatic adenocarcinoma diagnosed three months ago and not yet on therapy presented to the emergency room with symptoms of nausea, vomiting, and abdominal pain for one day. Computed tomography of the abdomen and pelvis showed splenic infarcts, bilateral renal infarcts, and increased size of hepatic metastases. On the second day of hospitalization, he developed confusion and aggressive behavior. Magnetic resonance imaging of the brain demonstrated multifocal acute infarcts scattered throughout the cerebral hemispheres bilaterally. Subsequent transthoracic echocardiogram and transesophageal echocardiogram showed a broad-based mitral valve vegetation. At that time, the differential diagnosis included infectious endocarditis or non-bacterial thrombotic endocarditis (NBTE). He was started on therapeutic enoxaparin and empiric antibiotic treatment. Blood cultures and other infectious evaluations that had been obtained remained negative. The presence of multiple systemic emboli, negative cultures, and presence of adenocarcinoma ultimately favored the diagnosis of NBTE over infectious endocarditis. Antibiotics were stopped and the case was discussed with oncology regarding the treatment of the underlying cancer. Unfortunately the patient remained intermittently confused and agitated with declining functional status despite being on anticoagulation. Oncology recommended against chemotherapy and he was transitioned to inpatient hospice care. Therapeutic enoxaparin was discontinued due to patient and family preference for comfort-only interventions, and he died four days later.
Discussion: Non-bacterial thrombotic endocarditis is a rare condition that is most often seen in the setting of advanced malignancy or connective tissue disease. This case of NBTE was diagnosed only after further investigation of infarcts that were incidentally found during evaluation of abdominal pain. NBTE is often difficult to diagnose due to its insidious nature. Patients often lack the classic symptoms of infectious endocarditis such as fever and murmurs. The initial abdominal pain was the only clue to the presence of NBTE in our patient. This case also highlights the challenges of anticoagulation in patients with life-limiting illnesses that confer poor prognoses. Evidence for anticoagulation is limited in this population due to the low incidence of NBTE. One could advocate for continuing anticoagulation to decrease the propagation of further emboli. On the other hand, there is increased risk of intracranial bleeding in patients with known cerebral infarctions. Hemorrhagic stroke should always be ruled out prior to starting anticoagulation.
Conclusions: In patients with adenocarcinomas, embolic phenomena from NBTE should be on the differential as a cause of new and nonspecific symptoms including abdominal pain. Prompt treatment with anticoagulation after ruling out hemorrhagic strokes can help decrease embolic events. Ultimately, treating the underlying malignancy early on is the best way to prevent complications of NBTE.