Background: Interprofessional Plan of Care Rounds (POCR) are an organized assembly of the following health care team members: physicians, nursing, case management, social work, physical therapy, pharmacy, and other ancillary services (Terra, 2015). The purpose of the rounds is for the group to concisely review each patient, his or her goals for the day, discharge plan, to offer individual expertise, and ensure that quality care is being provided (Terra, 2015). The evidence suggests that organizations have found that interdisciplinary POCR reduces readmissions, mortality rate, and length of stay. In addition, well executed POCR improves quality metrics, and increases satisfaction in all team members (Terra, 2015). The Joint Commission has cited communication and care planning as frequently identified root causes in sentential events (Ryan et al., 2017).At our Academic Medical center, geographic placement of patients has been a barrier to interdisciplinary rounds. Specifically, our Hospital Medicine services have patients on anywhere from four to ten different nursing units. Hospitalists were unable to attend more than one to two POCR daily. In order to address the geographical challenges and allow for the Hospital medicine teams to speak with multiple Interprofessional unit-based teams, the Hospitalist team, in partnership with hospital administration and nursing leadership, implemented a remodel of POCR.
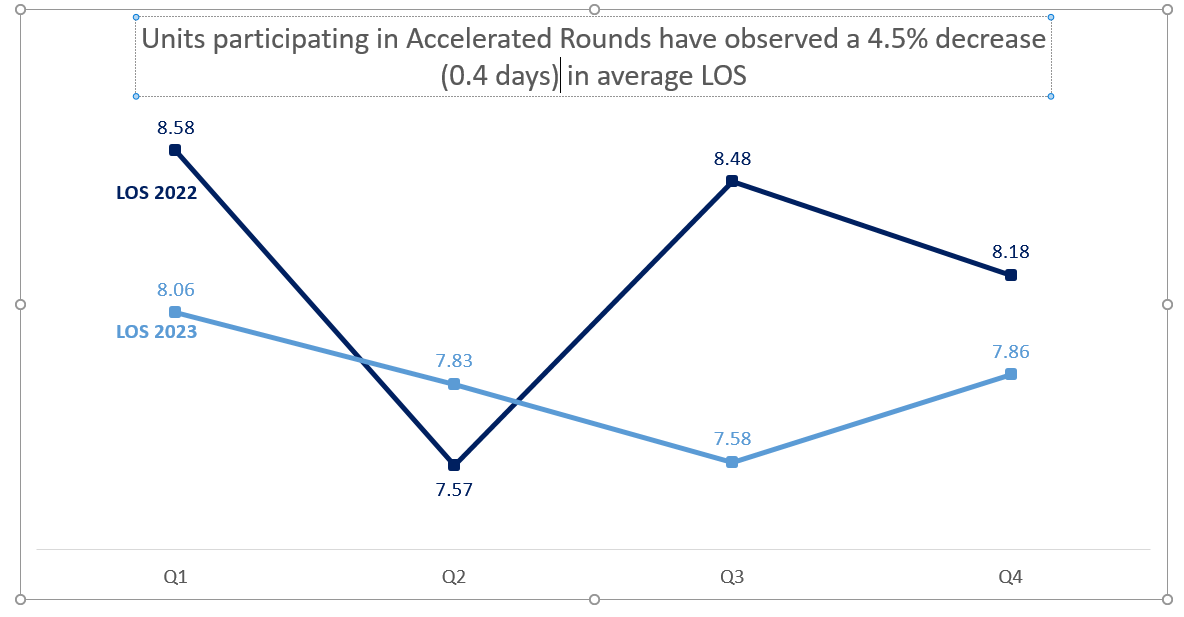
Purpose: The POCR were held in one central location for multiple units. We called the centralized rounds Accelerated Rounds. The goal was to maximize provider’s ability to attend rounds in person. Key performance indicators measured included: Length of stay, attendance by provider team, time per provider to complete rounds, total rime of rounds to be completed, and a qualitative assessment of the rounds by participants.
Description: In order to restructure the POCR and improve outcomes, unit-based nursing leaders were empowered as leaders of rounds and provided a structured training for POCR leadership, with the training lead by a Hospitalist Nurse Practitioner/ Director of Advance Practice Providers. A rounding checklist was refined and enforced at the training, and then brought to each unit by nursing and POCR leaders. Previous POCR start times were maintained, and other members of the interprofessional team: Physical and occupational therapy, and Case management/ social work continued to attend, but now in the new centralized location. Six nursing units participate in the initial phase, with two added within 2 weeks. Units were chosen based on percent of patients discharged by the Hospital Medicine teams. Twelve hospital medicine services, staffed by residents, advanced practice providers, and attending physicians, participated. A rapid-cycle PDSA process was followed for the first few weeks, with QR codes surveys distributed to collect feedback on the process.
Conclusions: Rounds take approximately 18 minutes per provider to complete, and 45 minutes overall to be done. Overall, a 4.5% reduction (0.4 days) in length of stay was achieved on these units. The percent of patients rounded on in person increased. In addition, the group noted other satisfactory outcomes including being well received by all members of the Interprofessional team, and overall increase in sense of community by participants. Opportunities to improve include adherence to checklist, improvement of closed loop assignment of barriers, and integration of more quality metrics into POCR discussions.