Background: In societies with an aging population, hospitalists manage patients with a multitude of comorbidities, and many have challenging social circumstances. Patients with high social risk tend to have poorer healthcare outcomes, yet it is unclear how prevalent social risk factors are among hospitalized patients. We studied the prevalence of social risk among hospitalized patients and its association with healthcare resource utilization and costs.
Methods: From October to December 2022, we conducted a physician-administered social risk questionnaire on patients admitted to an internal medicine ward in a tertiary hospital. We reviewed the literature on social determinants of health screened for by healthcare providers and researchers and created a questionnaire comprising 10 questions in the domains of education level, employment status, social connectedness, financial strain, housing security, access to transportation, as well as exposure to violence, stress, incarceration, and language difficulty. A significant social risk was defined as the presence of at least 2 out of 10 risk factors. We collected data on patients’ sociodemographic status, medical co-morbidities, their Clinical Frailty Scale (CFS) score, need for social services or a transfer to another institution on discharge and recorded their length of stay. We used multivariate logistic regression to determine the association of social risk with length of stay (LOS) using sociodemographic status, medical co-morbidities, CFS score, need for social services or transfer to another institution on discharge as covariates. To account for positive skew of LOS data, we used generalized linear modelling (GLM) to estimate excess costs due to social risk in terms of nominal bed-day costs.
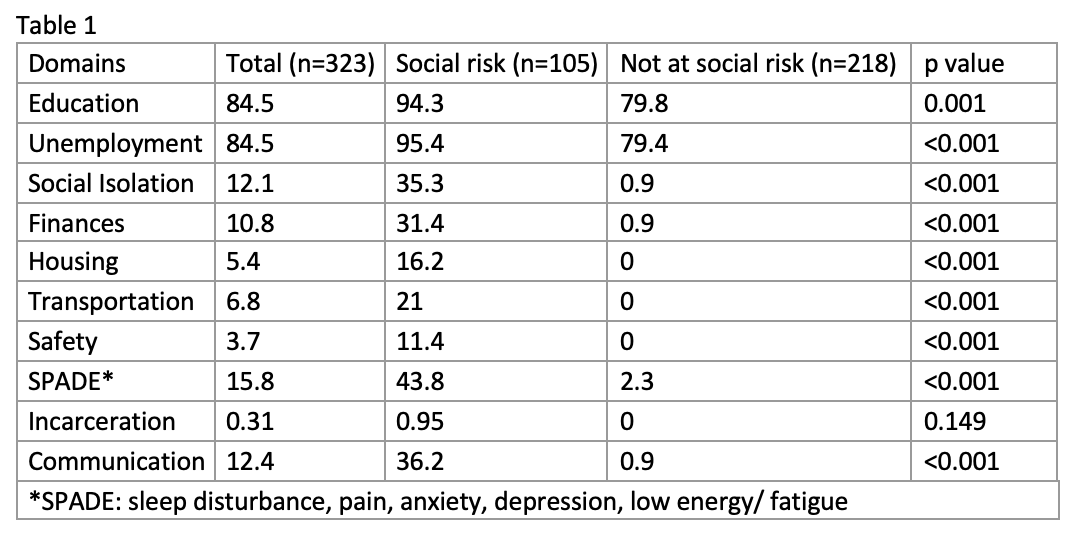
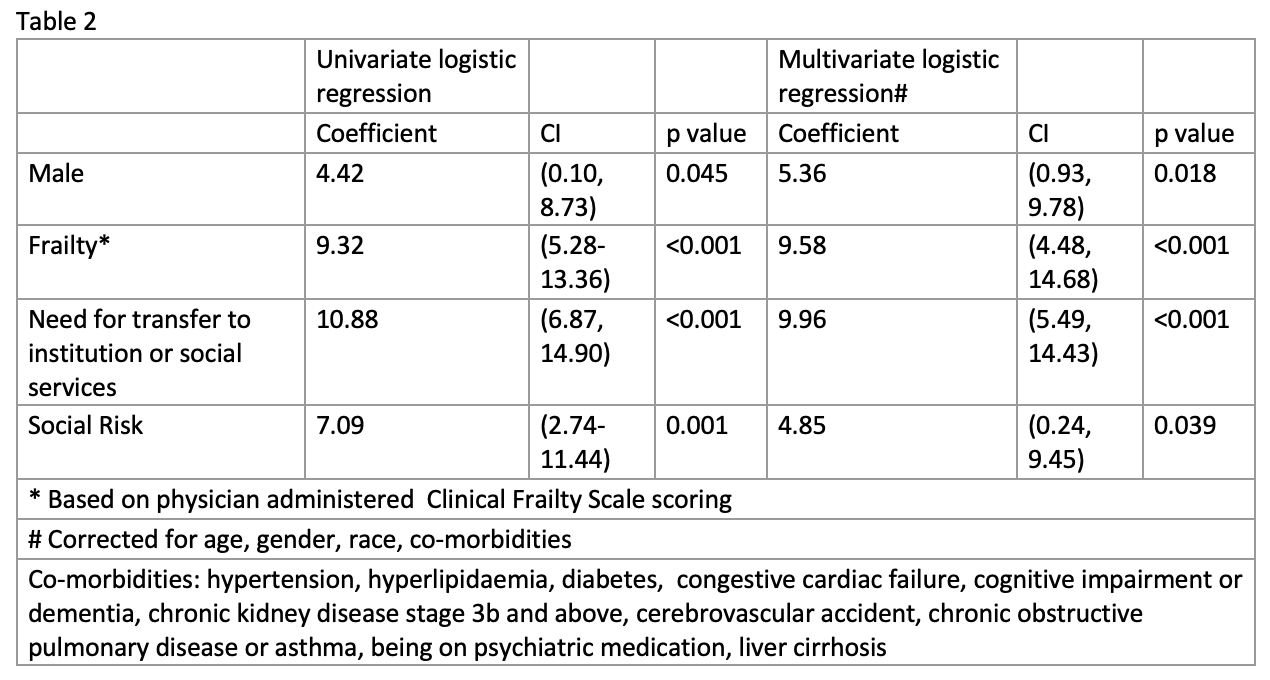
Results: A total of 323 patients were included in the study, with a mean age of 72.8 years (SD 14.4), 35% were male. 33% of our patients were identified as having significant social risk. This was independent of age. Patients identified as having social risk were more likely to be male, have a CFS score >3, have cognitive impairment or dementia, psychiatric disease, or chronic kidney disease (p-value< 0.05). Those identified as having significant social risk faced more isolation (35.3%, vs 0.9%, p-value < 0.001) (Table 1). They were more likely to have financial concerns (31.4%, vs 0.9%, p-value < 0.001), face issues with housing (16.2%, vs 0%, p-value < 0.001) and transport (21%, vs 0%, p-value < 0.001). 36% in the high social risk group had difficulties communicating with their healthcare provider, 11% had concerns for domestic safety, and 43.8% faced chronic stress, anxiety, low mood, or energy.Social risk was associated with prolonged LOS of 4.85 days (Table 2). Using GLM to model excess LOS based on nominal bed-day cost of USD (United States Dollar) 613, social risk was associated with an excess LOS of 2.45 days (CI 0.13 – 11.22), and USD 1505 (84-6879) per person per admission (excluding manpower and consumables cost).
Conclusions: There is a high prevalence of social risk factors in our inpatient population and it is associated with a prolonged LOS and higher healthcare utilization costs. Identifying social risk in hospitalized patients early can link them to target interventions to mitigate their social risk factors and enable them to achieve desired clinical outcomes, thereby increasing the value of care. This study paves the way for further research to develop guidelines for early identification of patients with high social risk factors.