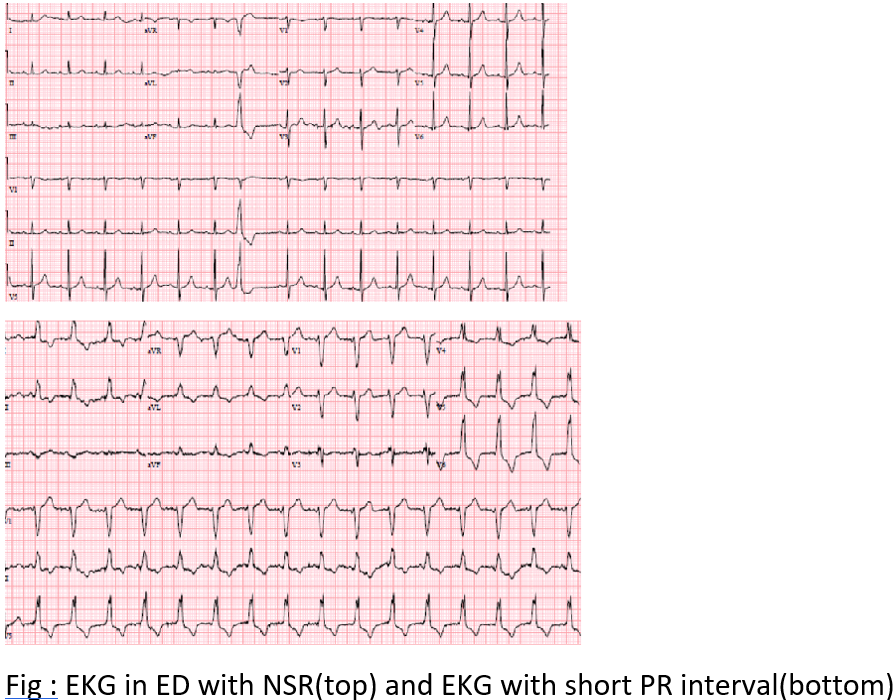
Case Presentation: 81 year old male with medical history of Abdominal Aortic aneurysm(AAA) ,COPD on home oxygen, diverticulitis post colon resection 10 years ago presented to the emergency department with painless hematochezia for 4 days. CT abdomen showed an interval increase in size of his AAA to 6 cm diameter and 8 cm in length with no causative finding for his gastrointestinal bleed .His Hemoglobin dropped from 12 to 10.1 and rest of the labs were normal . Initial EKG in ED was in normal sinus at 88 with intermittent premature atrial complexes and aberrant conduction of LBBB pattern. QRS complex and PR intervals were normal. The patient was admitted to hospital for evaluation of GI bleed and enlarging AAA . The following day, he had intermittent bleeding with borderline tachycardia and increased frequency of atrial ectopic on telemetry. A change in QRS morphology was noticed on telemetry and a repeat EKG was done which showed a new onset Left Bundle Branch Block (LBBB ) with sinus tachycardia at 108 and short PR interval of 56ms. The patient denied chest pain and was hemodynamically stable throughout. His cardiac enzymes were negative and transthoracic echo showed normal Left ventricular function with no wall motion abnormality . The same night, the patient had another episode of massive hematochezia. His hemoglobin dropped to 6.0 and he now developed a narrow complex tachycardia likely Atrio ventricular rentrant tachycardia (AVRT) at the rate 200bpm. His tachycardia terminated with adenosine to reveal normal sinus rhythm with normal QRS morphology . Cardiology was consulted, and made a diagnosis of right sided concealed accessory pathway with preferential retrograde conduction . The reason for transient anterograde conduction during acute stress could not be completely explained but assumed to be due to sympathetic overdrive and frequent atrial ectopic .He was transferred to the ICU and required multiple transfusions .The patient and family eventually wished for comfort care measures and expired shortly in a hospice facility
Discussion: In a critically ill patient development of LBBB is concerning for acute myocardial infarction .But here we are presenting a a case of rare but alternate explanation as the cause of it. Bypass tracts that conduct only in the retrograde direction occur with an incidence reported as high as 16 percent . Because they do not preexcite the ventricles, the surface EKG during sinus rhythm appears normal and therefore these pathways are called “concealed”. Some concealed pathways may be able to conduct anterograde, but have such long refractory periods that they do not conduct during sinus rhythm and are concealed. Preexcitation can sometimes be seen in patients with this type of a concealed accessory pathway after a long sinus pauses like atrial ectopics as seen in the above case Most concealed AV bypass tracts exhibit nondecremental conduction and, because they serve as conduit for retrograde ventriculoarterial (VA) conduction, they are associated with reentrant arrhythmias like in this case
Conclusions: Acute Left bundle branch blocks are commonly associated with ominous transmural myocardial infarction(MI) ,but if MI is ruled out we need to consider other clinically significant etiologies like concealed accessory pathways leading to cardiac arrhythmias