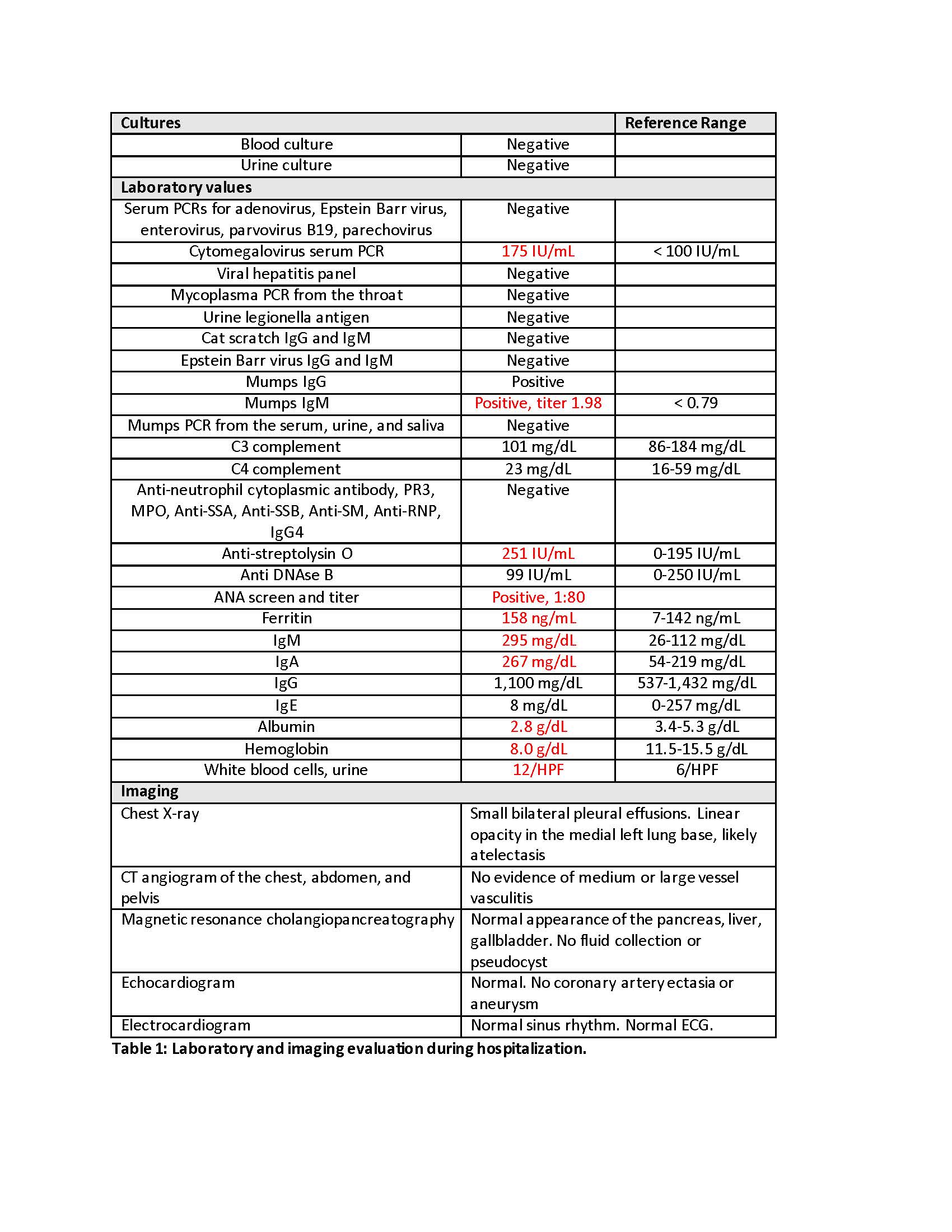
Case Presentation: A previously healthy 8 year old male presented to the emergency department (ED) with a one day history of diffuse abdominal pain, nausea, non-bloody and non-bilious vomiting, and fever up to 39˚C. Appendix ultrasound was normal. Urinalysis was significant for protein, ketones, and bilirubin. Influenza A/B PCR was negative. He improved with intravenous fluids and ondansetron and was discharged home. He returned to the ED later the same day due to worsening abdominal pain, continued fevers, and new rash. He was afebrile with age appropriate vital signs. His physical exam was significant for mild diffuse abdominal tenderness without rebound or guarding, left sided cervical lymphadenopathy (<1.5 cm), grade 2/6 vibratory systolic murmur, and an erythematous maculopapular rash covering the chest, back, arms, and legs. Laboratory evaluation on presentation was significant for AST 121 U/L, ALT 186 U/L, total bilirubin 1.7 mg/dL, direct bilirubin 1.4 mg/dL, GGT 245 U/L, lipase 257 U/L (reference range <202 U/L), white blood cell count 7.1 K/uL with increased bands and decreased lymphocytes, hemoglobin 10.9 g/dL, clumped platelets, erythrocyte sedimentation rate 53 mm/h, C-reactive protein 18.4 mg/dL, procalcitonin 1.6 ng/mL, group A strep throat swab negative, nasopharynx respiratory infection array negative, and repeat urinalysis positive for ketones. Abdominal ultrasound including evaluation of the liver, gallbladder, pancreas, spleen, and kidneys showed no abnormality. He was admitted for supportive care for presumed viral infection.He continued to have daily fevers up to 39-40.5˚C and abdominal pain. Repeat lipase was 1,964 U/L, and he was diagnosed with acute pancreatitis. He developed bilateral conjunctivitis. He underwent an extensive work up for infectious and inflammatory disorders (Table 1) which did not reveal a clear etiology. On day 9 of fever he was diagnosed with atypical Kawasaki disease based on meeting the clinical criteria of rash and conjunctivitis as well as supplemental laboratory criteria of anemia, elevated ALT, low albumin, and sterile pyuria. He received IVIG (2 g/kg) and high dose aspirin (80 mg/kg/day). Fevers and abdominal pain resolved. He transitioned to low dose aspirin 48 hours after resolution of fever. Abnormal laboratory values improved and eventually normalized. Follow up echocardiograms were normal. He stopped aspirin therapy 2 months after discharge.
Discussion: Pancreatitis in association with Kawasaki disease (KD) has been rarely reported in the literature. On review of 8 identified case reports, patients were more likely to be older (5-16 years of age) and male. Pancreatitis may indicate more severe disease, as 3 of the 8 patients had symptoms refractory to one dose of IVIG, and 3 of the 8 patients developed coronary artery aneurysms. In addition, two autopsy studies of KD found inflammation of the pancreatic parenchyma in 22-36% of subjects, suggesting a higher prevalence of pancreatic involvement in those with severe disease.
Conclusions: Although uncommon, in the appropriate clinical scenario KD should be considered in the differential diagnosis of acute pancreatitis in children. An evaluation for pancreatitis should be included in the work up of patients with KD and abdominal pain. Clinical pancreatitis may portend more severe disease, thus close follow up and monitoring after hospital discharge should be ensured.