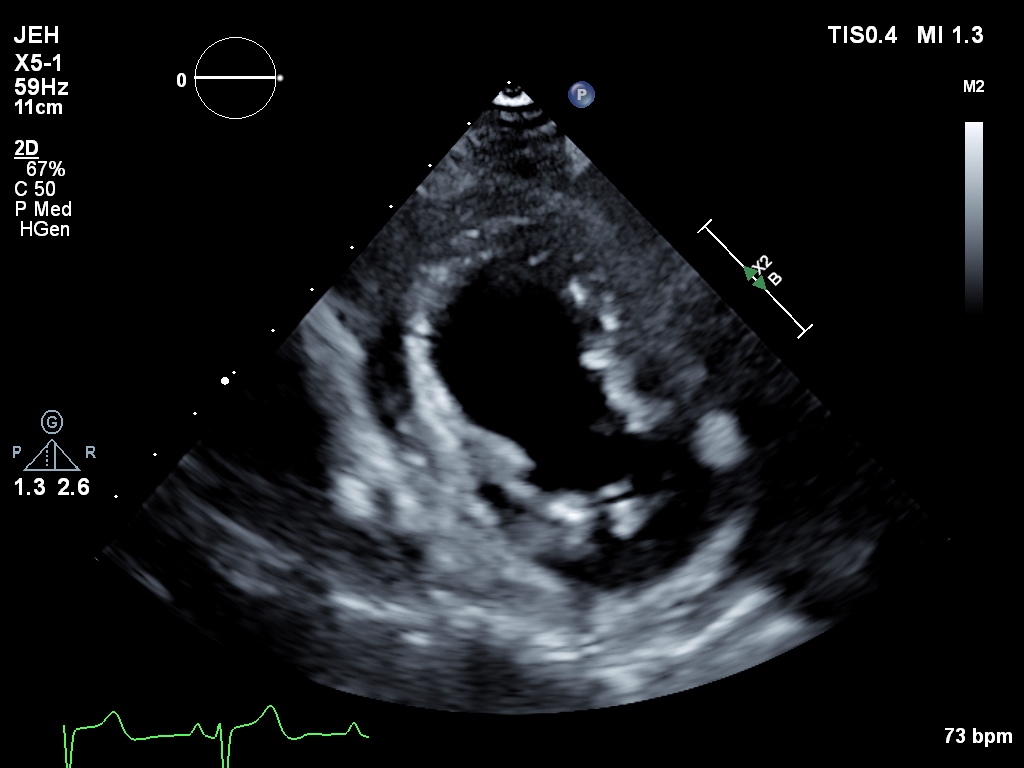
Case Presentation: An 85-year-old female presented to the emergency department in August of this year with acute chest pain and shortness of breath. The patient was afebrile, with a heart rate of 97 bpm, a respiratory rate of 24 breaths per minute, and a blood pressure of 191/81 mmHg. Labs showed hemoglobin of 6.6 g/dL and troponin of 4.6 ng/mL. An Electrocardiogram (EKG) revealed ST elevations in leads V1 and V2. A non-contrast CT chest and CTA of the chest, abdomen, and pelvis were unremarkable. An Echocardiogram revealed moderate tricuspid regurgitation and moderately elevated pulmonary artery systolic pressure of 45-50 mmHg. Due to concern for a ST-elevation MI ( STEMI), the patient was started on a heparin drip and transferred to the cath lab. The catheterization revealed a complex 90% lesion in the mid-left anterior descending artery (LAD), and a drug-eluting stent was placed. However, the procedure was complicated by dissection of the LAD. Immediately following the procedure, the patient became hypotensive and developed pleuritic chest pain. Labs revealed leukocytosis (12,900 cells/µL), a chest X-ray showed a left-sided pleural effusion, and a stat Echocardiogram revealed a large, anterior, loculated pericardial effusion. The patient was diagnosed with Post-Cardiac Injury Syndrome (PCIS) secondary to Percutaneous Coronary Intervention (PCI) and was started on Colchicine. Pericardiocentesis was performed and 200mL fluid was drained. Once the pericardial effusion resolved, the pericardial drain was removed, and the patient was discharged in a hemodynamically stable condition.
Discussion: Postcardiac Injury Syndrome (PCIS) is an umbrella term that includes post-pericardiotomy syndrome, post-myocardial infarction-related pericarditis (Dressler syndrome), and post-traumatic pericarditis, which can be either iatrogenic (resulting from procedures like percutaneous coronary intervention [PCI]) or non-iatrogenic (following blunt or penetrating trauma) [1]. It is characterized by inflammation of the pericardium, pleura, and pulmonary parenchyma following cardiac injury. PCIS most commonly results from major cardiac surgeries (about 15% of cases) while PCIS following PCI occurs in only about 0.5% of cases [2], an incidence that has decreased with the advent of minimally invasive techniques.Diagnosis is based on a recent history of pericardial injury and the presence of at least two of the following five criteria: unexplained fever, pericardial or pleuritic chest pain, pericardial or pleural rubs, pericardial effusion, and pleural effusion with elevated CRP [3]. Pleural effusion in PCIS results from the contiguous spread of pericardial inflammation or simultaneous pleural injury. It usually develops weeks after injury, but it can appear acutely in rare cases [4], as seen in this case. Hospitalists should maintain a high index of suspicion in patients with recent cardiac procedures, as early identification can improve outcomes and reduce morbidity.
Conclusions: This case underscores the importance of recognizing early signs, such as pleural and pericardial effusion, which may develop days to weeks after cardiac injury but can present acutely, as seen in this patient. Hospitalists should remain vigilant in monitoring for and managing cardiac procedure-related complications, ensuring timely interventions to improve patient outcomes.