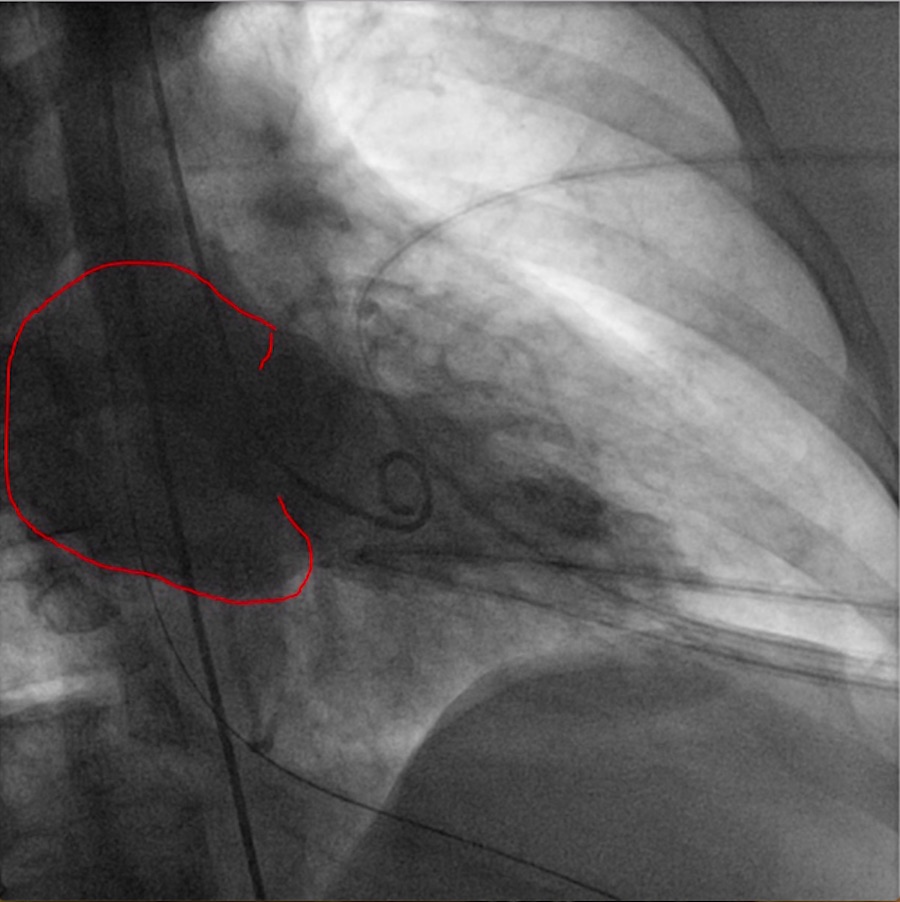
Case Presentation: We describe an interesting case of a 59-year-old female patient who arrived unresponsive to ED, with symptoms concerning for acute coronary syndrome(ACS). There was no informant present along with the patient, so very limited information was available about patient’s past medical history or risk factors. EMS personnel who accompanied the patient reported that patient was complaining of some chest and back pain before she was brought unresponsive, cyanotic with agonal breathing. Pulse was lost shortly after arrival with pulseless electrical activity (PEA) in 50’s on monitor. Patient was aggressively resuscitated with bag mask ventilation, high quality chest CPR, multiple rounds of epinephrine and atropine for bradycardic PEA and transient bradycardia. Review of initial EMS EKG showed anterolateral STEMI and cath lab was activated. Initial bedside echo showed poor contractility. Patient had several episodes of ventricular tachycardia responsive to defibrillation, treated with amiodarone. Once perfusion was restored patient was placed on epinephrine drip. Repeat EKG showed wide irregular rhythm with ST segment elevation (STE) in V3. Patient had emergent cardiac catheterization, which showed severe three vessel disease with over 90% stenosis in all three vessels, acute thrombotic occlusion of the proximal left anterior descending (LAD) artery, anteroapical dyskinesis and severely reduced left ventricle ejection fraction, diffuse disease in the abdominal to pelvic aorta and in the left iliac artery precluding intra-aortic balloon pump implantation. Successful angioplasty and stenting of the proximal LAD using 3.0 x 18 mm bare metal stent was done. Patient was taken to the intensive care unit and emergent echocardiogram was ordered, however, patient arrested again with PEA. Patient had significant hemodynamic and electrical instability requiring maximum pressor support before and after procedure, but unfortunately passed away due to cardiogenic shock following severe mitral regurgitation most likely due to papillary muscle rupture
Discussion: Acute papillary muscle rupture occurs in less than 1% of patients with acute myocardial infarction and represents about 5% of all cases of ischemic regurgitation, with papillary muscle rupture carrying around 80-90% mortality. Most physicians rely on transthoracic echocardiogram (TTE) for the diagnosis of severe mitral regurgitation, but transesophageal echo (TEE) can be equally helpful in critically ill patients as it is sometimes difficult to get optimal window due to mechanical ventilation or restrictions in optimal positioning. Emergent surgical intervention is indispensable in acute MR with papillary muscle rupture, however, chronic mitral regurgitation patients can opt for newer modalities with transcatheter edge-to-edge repair.
Conclusions: Severe mitral regurgitation due to a ruptured chordae or papillary muscle rupture can be a fatal complication following acute myocardial infarction. Mitral valve surgery remains as a mainstay of treatment in emergent cases. Despite improvement in surgical and revascularization strategies, high mortality remains a major sticking point. Time is of paramount importance, so diagnostic confirmation should be done rapidly and definitively. Emergent medical therapy should be initiated immediately after diagnosis is confirmed with subsequent referral to surgery without delay.