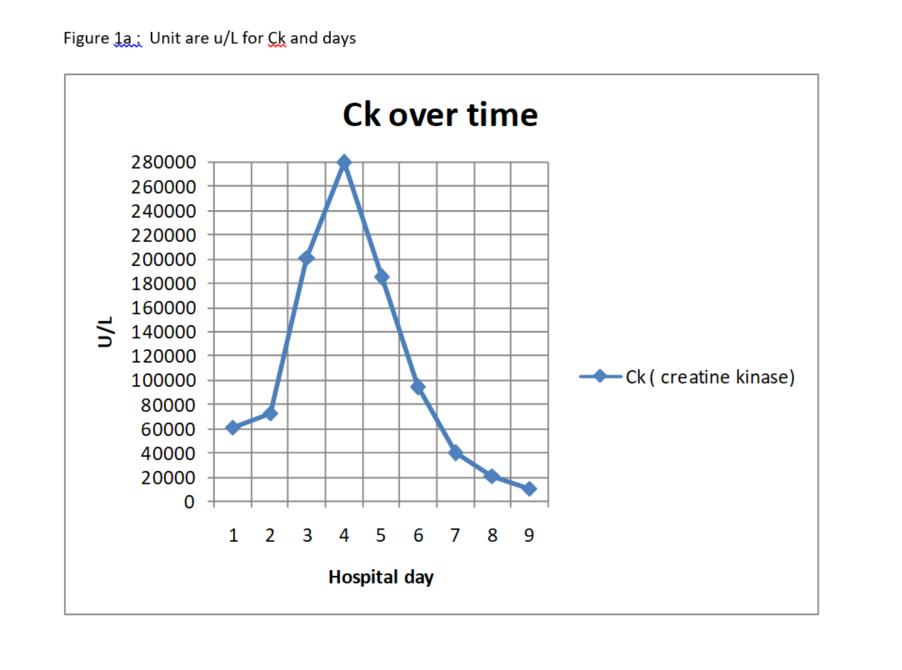
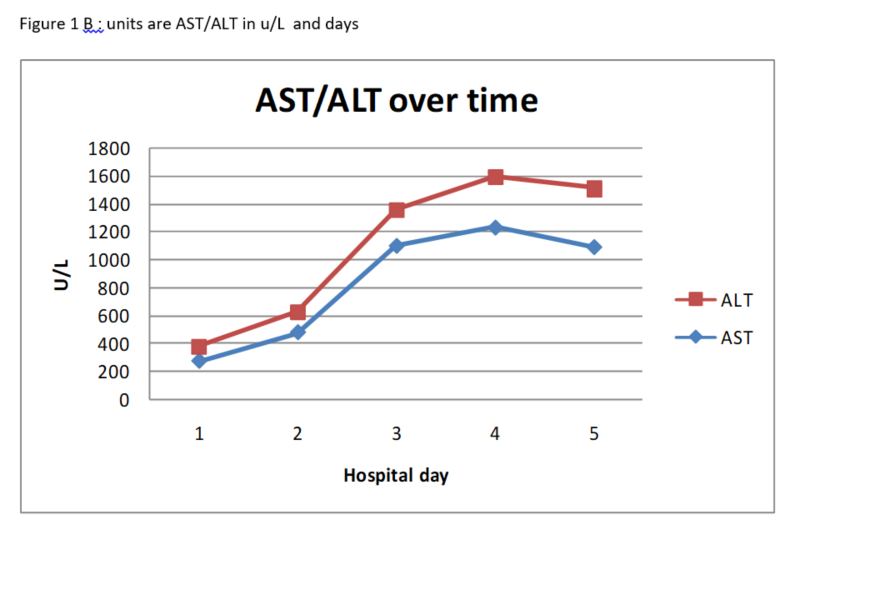
Case Presentation: A 41-year-old African American male with a past medical history of overactive bladder and benign prostatic hyperplasia presented to the emergency department (ED) with increasing proximal bilateral lower extremity muscle pain for five days. His pain was accompanied with increasing difficulty with ambulation. The patient also noted persisting hematuria, urgency, and hesitancy for the preceding nine days. Prior to presentation at our ED, the patient was diagnosed with a urinary tract infection (UTI) and prescribed Trimethoprim-Sulfamethoxazole (TMP-SMX). On exam, the patient appeared grossly uncomfortable. He was found to have lower extremity proximal muscle weakness without point tenderness. Abdominal exam was significant for mild left lower quadrant and suprapubic tenderness to palpation. Physical exam was otherwise unremarkable. Initial laboratory analysis in the ED showed an AST 274 u/L, ALT 102 u/L, CK-MB 3.11 u/L with a CK 60665 u/L. Prior outpatient labs showed normal transaminases and a urinalysis consistent with a UTI, but no laboratory evidence of rhabdomyolysis prior to initiation of TMP-SMX. In the ED, the patient received intravenous ceftriaxone and normal saline and was admitted to the inpatient medicine service with a concern for non-traumatic acute rhabdomyolysis and pyelonephritis. Studies to identify alternate etiologies for rhabdomyolysis were negative, including influenza screen, HIV, and drug toxicology. Epstein Barr viral studies were consistent with a prior infection, without evidence of an acute viral process. Thyroid function tests and Glucose-6-Phosphate dehydrogenase studies were also normal.
Discussion: The etiology of the rhabdomyolysis is varied and may be the result of toxin-mediated mechanisms, metabolic derangements, or may develop secondary to other conditions like seizures, trauma and prolonged immobilization. To our knowledge, this is only the fourth published case of TMP-SMX induced rhabdomyolysis in a patient without HIV infection. Our case adds to the growing body of literature suggesting TMP-SMX as a cause of possible drug induced rhabdomyolysis.
Conclusions: We present a patient with suspected acute toxin-mediated rhabdomyolysis in the setting of new Trimethoprim-Sulfamethoxazole therapy for urinary tract infection. The patient underwent a comprehensive evaluation for several other possible causes of rhabdomyolysis including influenza, HIV, drug use, trauma, and even inborn errors of metabolism. Considering the lack of alternate identifiable causes of muscle injury and the clinical improvement after discontinuation of TMP-SMX, we conclude that TMP-SMX was likely the insulting agent.