Background: Hospitalizations for opioid overdose and complications of opioid use disorder (OUD) have risen dramatically over the last two decades. Hospitalizations represent opportunities to initiate lifesaving medications for OUD (MOUD), but rates of hospital MOUD initiation are low. Addiction consult services (ACS) can help facilitate hospital MOUD initiation and promote linkage to post-discharge MOUD, but few studies have rigorously examined ACS outcomes specifically for patients with OUD. We aimed to determine the association between an ACS consultation and the provision of MOUD during admission, at discharge, and linkage to post-discharge MOUD.
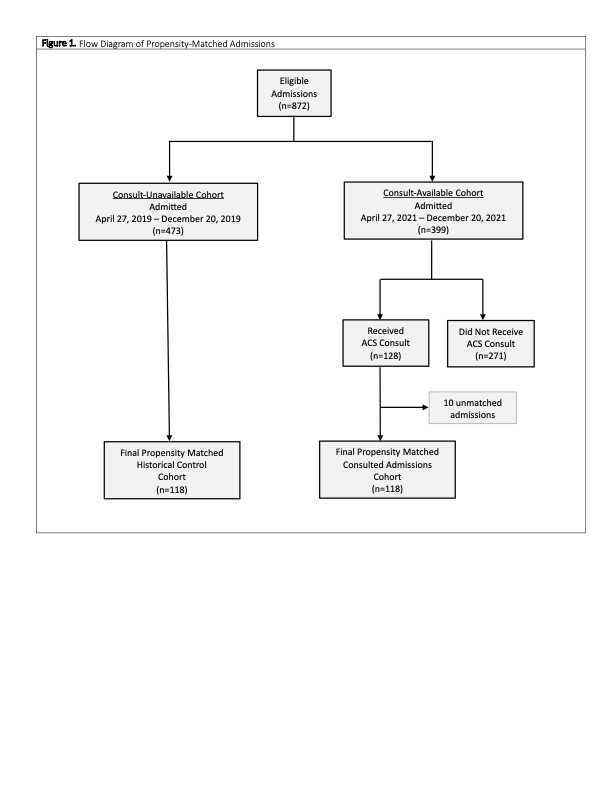
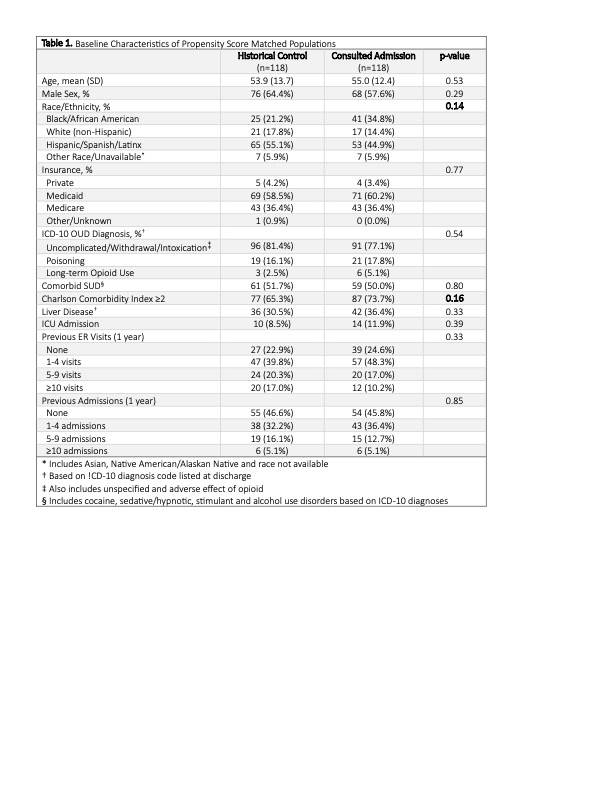
Methods: We used a retrospective propensity score-matched historical control design to evaluate the effect of ACS consultation on inpatients with an opioid related diagnosis. The ACS is an interdisciplinary service which includes a board-certified addiction medicine attending physician, an addiction medicine fellow, and peer advocate. Each admission with an opioid related diagnosis who received an ACS consult was matched with a control admission from the historical, consult-unavailable time-period. The propensity score was determined by a non-parsimonious 25-variable model including demographic, clinical and admission-level covariates. The primary outcomes were provision of MOUD during admission and at discharge (either prescription for buprenorphine or linkage to outpatient methadone treatment). Secondary outcomes included: patient-directed discharge, 30-day readmission, and 30-day post-discharge ER visit. Unadjusted and adjusted associations between consultation and each of the outcomes were determined using univariable and multivariable logistic regression.
Results: Among hospitalizations with an opioid use related diagnosis, there were 118 admissions who received an ACS consultation matched with 118 historical controls yielding a study sample of 236 admissions. Admissions receiving an ACS consult were significantly more likely to receive inpatient MOUD compared to historical controls (61.0% vs 30.5%, OR 3.57 [CI 2.05-6.19], AOR 4.35 [CI 2.35-8.07]). There was a significantly greater likelihood for those receiving a consult to be prescribed buprenorphine at discharge compared to control admissions (28.8% vs 0.9%, OR 47.36 [CI 6.33-354.08], AOR 46.65 [CI 5.94-366.10]). Consultation also had a significant association with linkage to outpatient methadone treatment compared with control admissions (5.8% vs 0.9%, p=0.03). ACS was not associated with reduced patient-directed discharge, 30-day readmission, or 30-day post-discharge ER visit.
Conclusions: ACS consultation was associated with a large increase in inpatient provision of MOUD and prescription or linkage to MOUD at discharge when compared to propensity-matched historical controls. These findings suggest the compelling benefit of an interprofessional ACS to provide evidence-based treatment for OUD.