Background: Conducting early serious illness conversations (SICs) is a high-value intervention that improves the patient and family experience while aligning care with patient preferences. Given the constraints of hospital-based clinicians, using the EHR to identify appropriate patients for SICs remains a key challenge. The aims of this study were to explore whether the EHR’s readmission risk score (Epic Systems, Inc.) identifies patients who might benefit from a SIC during hospitalization, and to perform a quantitative and qualitative analysis of documented SICs.
Methods: We conducted a retrospective analysis of adult patients admitted to the general medicine service of a community teaching hospital affiliated with an academic medical center from October 2018 to July 2019 who had an SIC documented in the EHR during hospitalization. We used our enterprise data warehouse (EDW) to obtain patient demographics, the readmission risk score at the time of admission, length of stay (LOS), palliative care consult orders, code status at discharge, discharge disposition, and structured SIC entries. We conducted a thematic analysis of two open-ended SIC items: 1) what is important to the patient and family, and 2) recommendations or next steps in management.
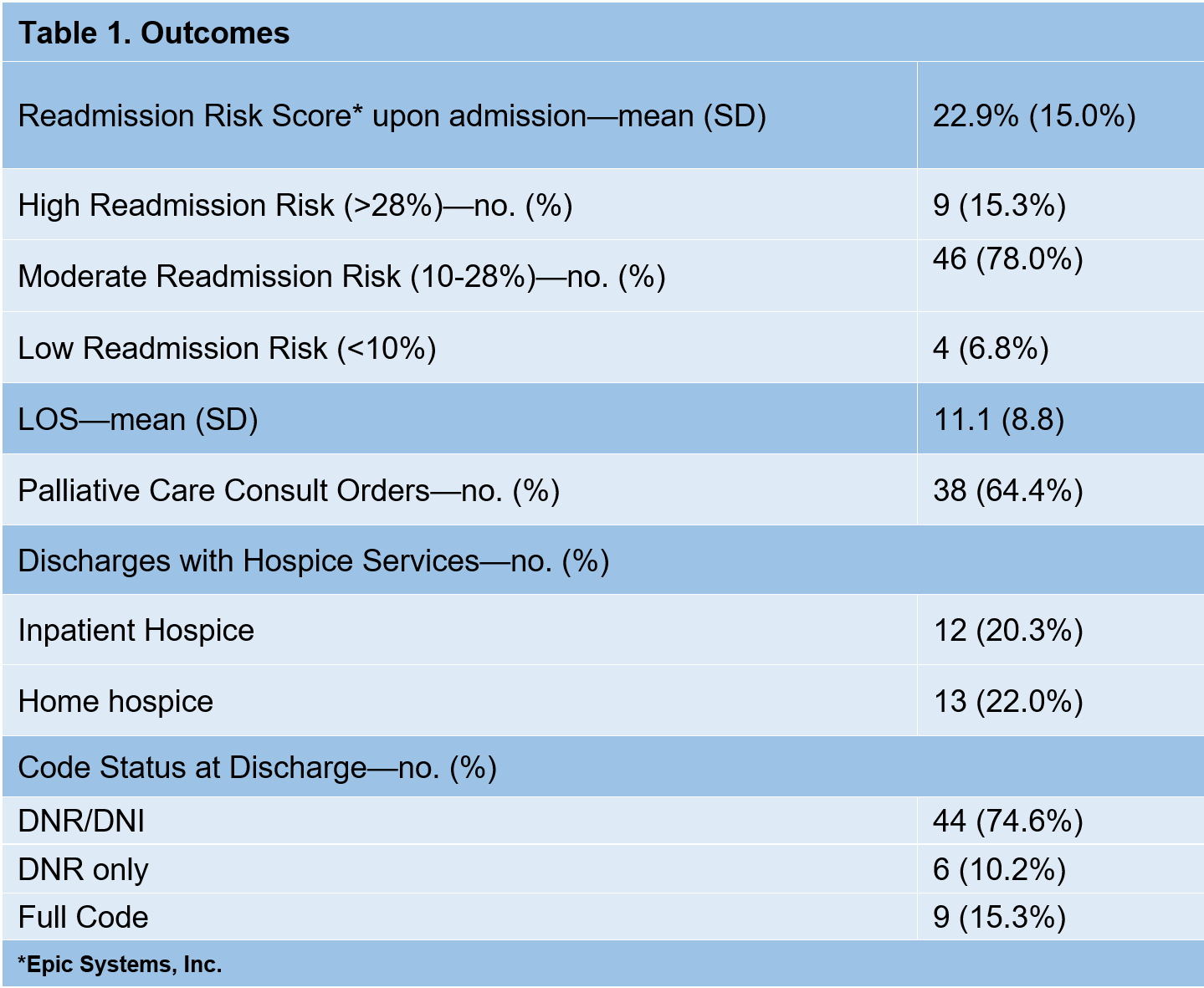
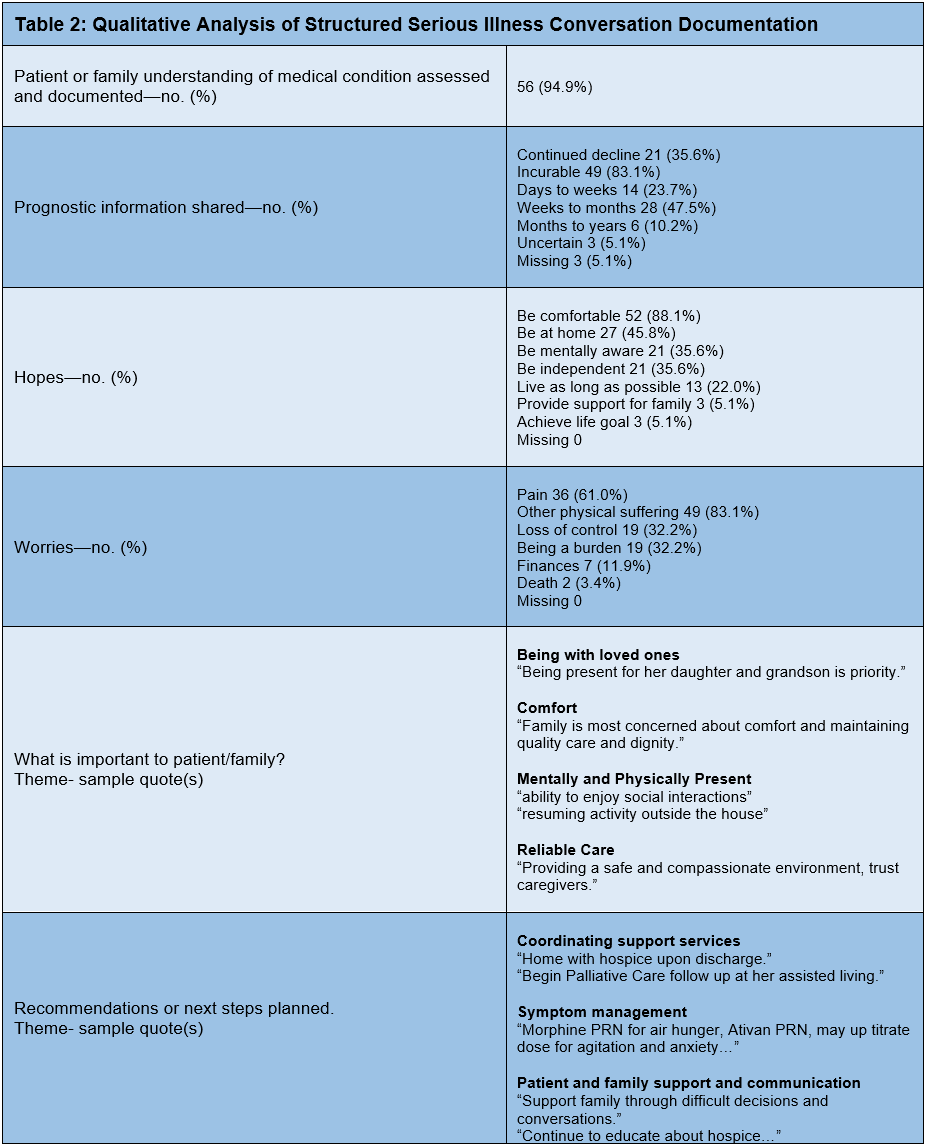
Results: We identified 59 unique patients with structured SIC documentation: 40 (67.8%) female; mean (SD) age 83 (11) years; 39 (66.1%) Caucasian; 43 (72.9%) Non-Hispanic; 46 (78%) public insurance; mean (SD) Elixhauser comorbidity score 5.6 (2.1). The mean (SD) readmission risk score (Table 1) was 22.9% (15): 55 (93.2%) patients had moderate (10-28%) to high (>28%) readmission risk. At discharge, 50 (84.7%) had a code status of DNR/DNI or DNI alone, and 25 (42.3%) had hospice services. In 56 (94.9%) cases (Table 2), clinicians documented patient (or family) understanding of the medical condition(s). Documented prognostication revealed incurable disease in 49 (83.1%), with either days to weeks or weeks to months left to live in 14 (23.7%) and 28 (47.5%), respectively. The most common hope was being comfortable in 52 (88.1%) patients. Most common worries were pain and other physical suffering in 36 (61.0%) and 49 (83.1%) patients, respectively. Major themes regarding what was important to the patient and family included: being with loved ones, comfortable, mentally and physically present and having reliable care to keep patients safe. Major themes regarding next steps included: coordinating support services; symptom management; patient/family support and communication. Life-sustaining treatments were minimally discussed.
Conclusions: In this study, patients with a structured SIC documented during hospitalization had moderate to high readmission risk scores and had high use of palliative care consultations and hospice services at discharge. Most patients had documented clinician prognoses ranging in days to months of life, indicating that those conversations we studied occurred possibly quite late in life. These findings suggest that patients might benefit from SIC’s that are initiated earlier in the disease course. Themes of SICs indicated that many patients and families do not want aggressive hospital care at the end of life; earlier knowledge of, documentation of, and adherence to these wishes could make a big difference for patients and families. While the readmission risk score could be a useful screening tool, other EHR prediction tools (frailty index, annualized mortality risk) may help to further stratify and identify patients who benefit from SICs.