Background: Work schedules are an important contributor to clinician satisfaction and wellbeing. Following increased work demands from the pandemic, we implemented a change to our hospitalist service structure from a “standard model” with 12-hour, 7-day on, 7-day off shifts including both rounding and admitting duties to an “admitter rounder model” which consisted of primarily 10-hour day rounding shifts and separate 10-hour admitter shifts. Two of the 7 hospitalist rounding services remained the standard 12-hour shifts though without admitting responsibilities.
Purpose: We sought to improve physician and advanced practice provider (APP) work/life satisfaction through changes to the hospitalist service structure. To assess the impact on quality of patient care we examined the changes in readmission rates and overall length of stay (LOS) for patients on the hospitalist services compared to all hospitalized patients.
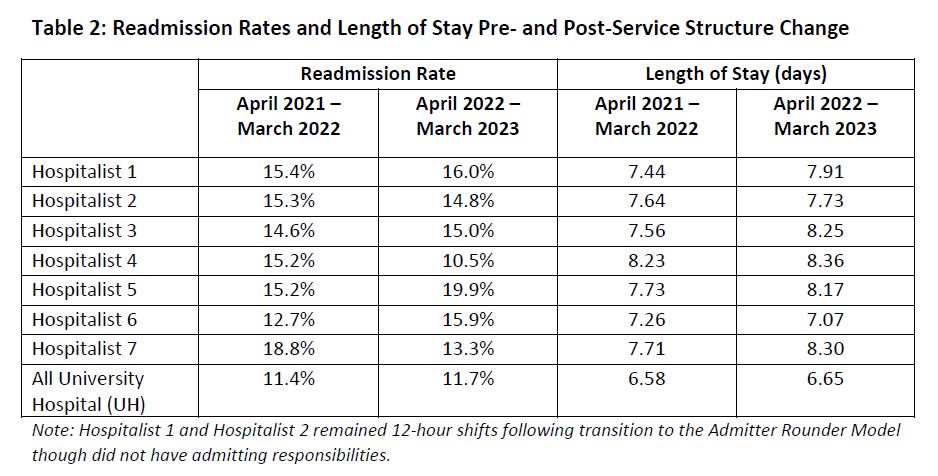
Description: On April 5, 2022, we transitioned from the standard model to the admitter rounder model. Hospitalist physicians (n=28) and APPs (n=8) were surveyed 6 months later in October of 2022 on their experience following implementation of the admitter rounder model (Table 1). Among physicians, 22 (78.6%) reported an improvement from the prior model, 2 (7.1%) reported no improvement, 3 (10.7%) did not work in the prior model, and 1 (3.6%) did not answer. Fifteen physicians (53.6%) reported fewer days feeling exhausted upon leaving work while 8 (28.6%) did not. Sixteen physicians (57.1%) felt the benefit of signing out at 5pm outweighed working more shifts overall while 10 (35.7%) did not. All 8 APPs reported an improvement from the prior model. Seven APPs (87.5%) reported fewer days feeling exhausted upon leaving work while 1 (12.5%) did not.We then retrospectively compared the change in readmission rates and LOS during the 12 months preceding the change (April 2021 to March 2022) to the 12 months after implementation (April 2022 to March 2023). We reviewed this for the 7 hospitalist services and compared this to the readmission rates and LOS among all hospitalized patients at University Hospital (UH) (Table 2). Patients primarily managed on hospitalist services account for approximately one-fifth of all hospitalized patients at UH. Among individual hospitalist teams, readmission rates variably increased or decreased; however, in aggregate, readmissions rates increased from 15.1% to 15.2%. During the same interval, readmission rates for all hospitalized patients at UH also increased from 11.4% to 11.7%. Hospital LOS increased among all but one hospitalist service during the comparison period as did overall LOS among all hospitalized patients at UH.
Conclusions: Compared to overall hospital operations during this time, changes to our hospitalist model did not result in increased readmissions or LOS. This is an early study to ensure changes to our model did not have any negative impact on hospital operations. Further work will be done to continue to evaluate patient safety, provider satisfaction, and impact on hospital workflows.