Background: In graduate medical education, learning to provide critical feedback is a key component of developing clinical competence, professionalism, and effective team-based practice. The role of the supervising resident in offering feedback to junior learners is particularly challenging because of the near-peer relationship and the lack of formal training on this skill. Simulation is an effective method of training that has been utilized to teach aspects of clinical care including clinical reasoning and team leadership.
Purpose: To increase confidence and improve performance among supervising residents in providing constructive resident-to-resident feedback by designing a novel, resident-led and facilitated case-based simulation session to practice delivering constructive feedback.
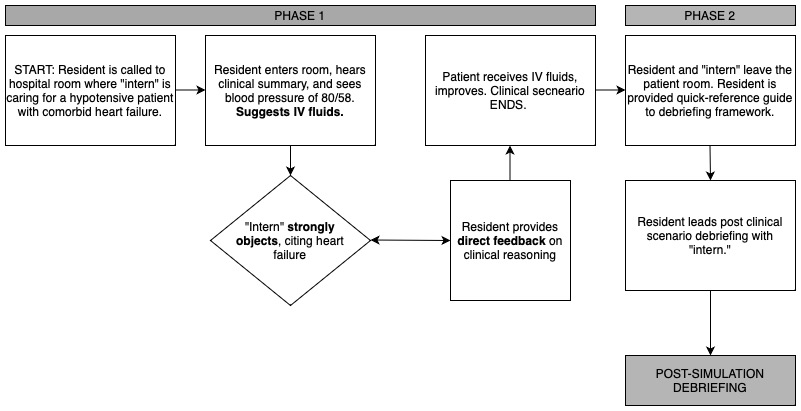
Description: In Spring 2023 we conducted a focus group of four medicine residents at different years in training to review perceived learning gaps in delivering feedback. Identified gaps were then converted into goal learning objectives as follows: 1. recognize the need to deliver resident-to-resident feedback in an acute medical scenario, 2. provide direct, clear, and respectful in-person feedback to a near peer learner during an acute medical scenario, 3. conduct an effective post-scenario debriefing session, and 4. utilize the Debriefing with Good Judgment framework, a previously published advocacy-inquiry style of medical simulation debriefing, for providing resident-to-resident feedback. Following this, we convened a working group consisting of the medicine residency simulation faculty lead, PGY2 and PGY3 medicine residents, and the simulation center education director to meet bimonthly from Spring 2023 to Fall 2023 to generate a draft simulation-based curriculum. During development, iterations of the case-based simulation were tested and refined with a focus on balancing the need to prompt the learner to take desired actions (e.g. to begin delivering feedback, to ask for a certain medical therapy) with the need to ensure psychological safety and preserve an element of surprise which is important in enhancing the fidelity of the simulation. For example, the intern’s objection to the resident’s suggested medical therapies needed to be sufficiently intense to prompt the learner to deliver direct feedback but not so intense as to cause undue interpersonal distress. After iteratively refining the simulation curriculum in this manner, the working group generated the final pilot case-based simulation curriculum (Figure 1).
Conclusions: Using key stakeholder feedback and leveraging simulation-based training, we have successfully developed and piloted a novel, resident-led simulation curriculum on the delivery of resident-to-resident feedback. Future directions include assessment of perceived confidence of learners following this session as well as direct observation of feedback performance.