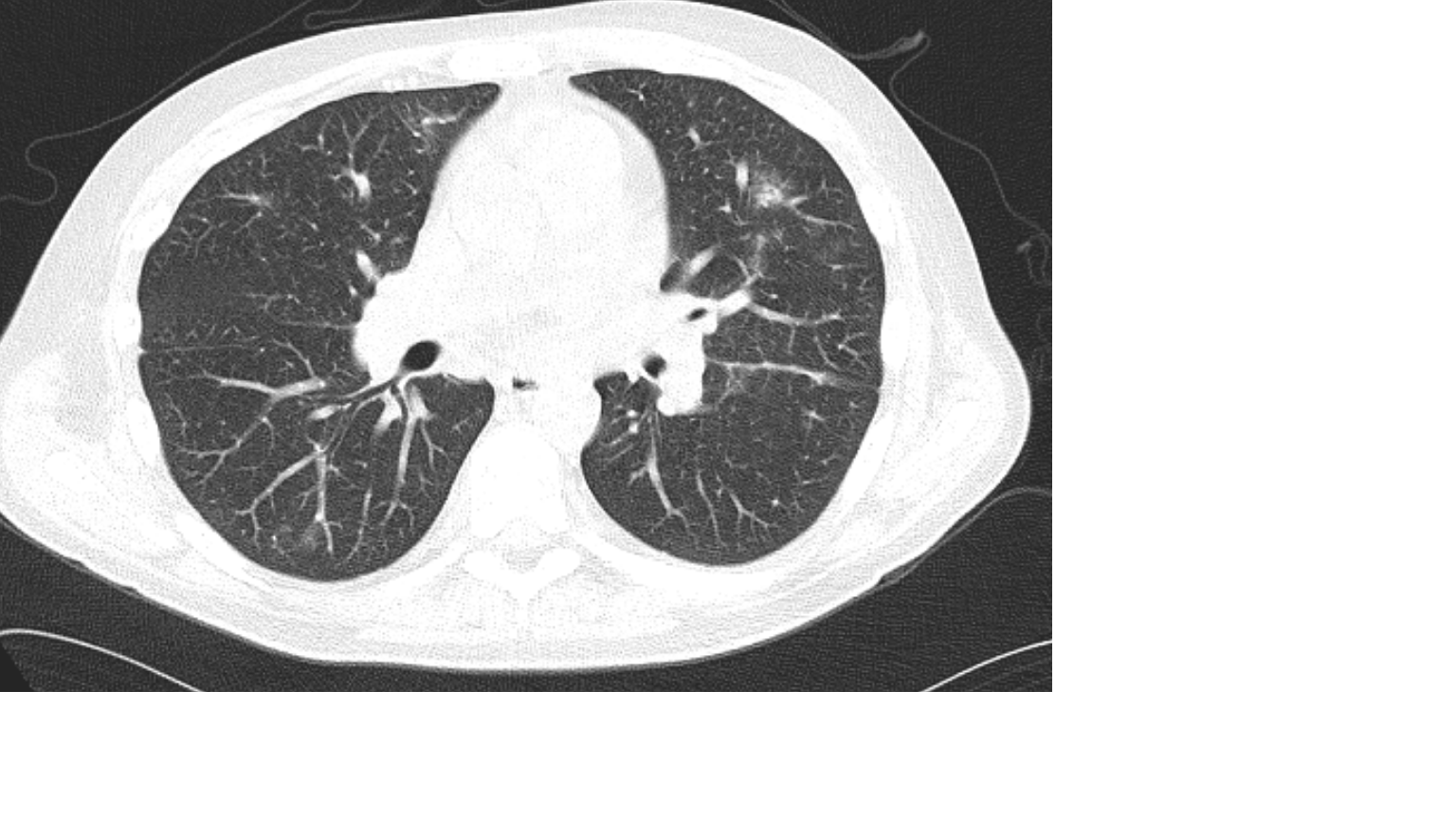
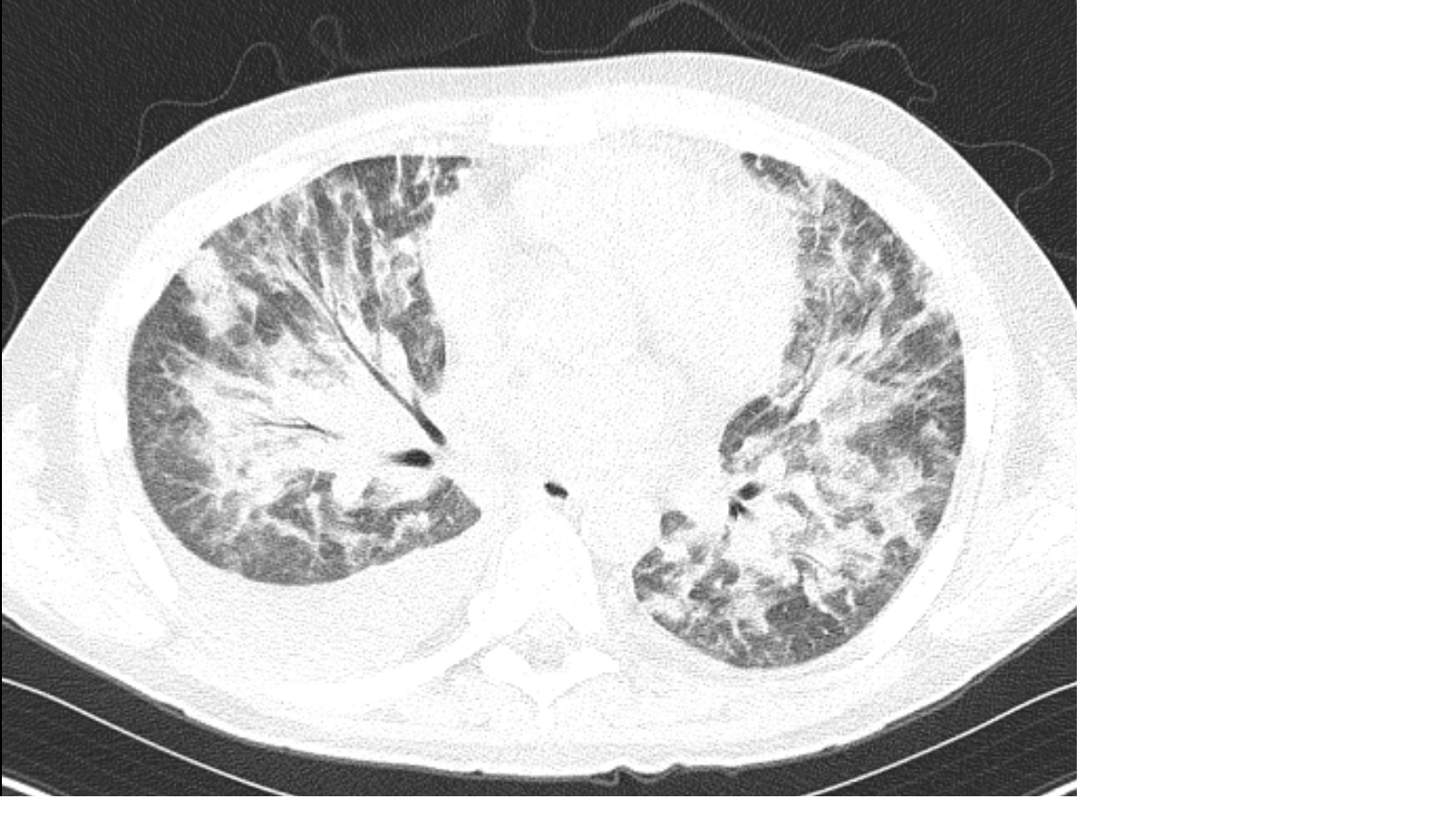
Case Presentation: A 28-year-old male with alcohol use disorder presented with 3 months of jaundice, arthralgias, and abdominal pain. His history raised concern for alcoholic hepatitis; his Maddrey’s score was 64.7. He initiated high dose steroid therapy. A calculated Lille score indicated that he would be responsive to steroids, and he was ultimately discharged on high dose steroids with a prolonged taper. His symptoms persisted, however, and he was readmitted a month later. He developed a mild, nonproductive cough along with dyspnea without hypoxia. Initial CT demonstrated mild ground glass opacities (GGOs). Despite empiric antibiotic therapy, the patient worsened, developing hypoxia and hemoptysis. A full infectious panel, including fungal serologies, was sent. His beta-D-glucan level was markedly elevated. Repeat imaging demonstrated significantly worse airspace disease and GGOs. PJP pneumonia was suspected. He was empirically started on Bactrim but developed acute respiratory distress and was intubated. BAL was positive for P. jirovecii. Despite treatment, the patient unfortunately passed.
Discussion: The typical presentation of PJP is dry cough, progressive dyspnea, and low-grade fever. In immunocompromised, HIV-negative patients, the onset of symptoms is much quicker: 5-6 days compared to 3-4 weeks for HIV-positive patients. AH can cause immunosuppression through immune system dysregulation by activating inflammatory pathways, which lead to exhaustion and a compensatory immunosuppressed state. In HIV patients, BAL can provide a much higher diagnostic yield due to the higher fungal burden in the lungs. PJP prophylaxis is commonly indicated in HIV patients with CD4 counts under 200. In other conditions, indications for PJP prophylaxis are more unclear, as in this presentation. Overall, this case represents a rare documented presentation of PJP in severe alcoholic hepatitis in someone on corticosteroid therapy without primary PJP prophylaxis.
Conclusions: Pneumocystis jirovecii pneumonia (PJP) is a common opportunistic fungal infection. In patients with HIV, the clinical presentation of PJP is well documented. PJP in HIV-negative, immunosuppressed patients is not as well studied. In those populations, PJP is associated with worse symptoms and higher mortality. Chronic steroid use is a common cause of immunosuppression, and typically necessitates prophylaxis for PJP. A less considered etiology for immunosuppression is acute liver failure, such as alcoholic hepatitis (AH). Severe AH is associated with a mortality as high as 30% at 28 days. PJP in patients with alcoholic hepatitis is rare. Here, we described a case of PJP in an HIV-negative patient with alcoholic hepatitis undergoing treatment with high dose steroids.