Case Presentation: Significant alcohol consumption can lead to a variety of alcoholic liver diseases ranging from alcoholic fatty liver disease to alcoholic hepatitis. Here, we discuss an atypical presentation of alcoholic hepatitis in a patient initially thought to have a hematologic malignancy.
Our patient was a 28-year-old Cantonese-American man presenting with one month of fevers, night sweats, malaise and an unintentional ten pound weight loss. He reports being a social drinker, having one beer every few months. Travel history was notable for a recent trip back to Asia. Physical exam revealed tachycardia, mild abdominal tenderness, hepatosplenomegaly, ascites, maculopapular rash on his extremities, and jaundice with no stigmata of chronic liver disease. Labs revealed a white blood cell count of 22×103/uL, AST 77, ALT 54, conjugated hyperbilirubinemia with a total bilirubin 4.4 mg/dL, alkaline phosphatase of 183 U/L, and an INR of 1.43.
Discussion: Given his recent travel, there was an initial concern for infection. However, an infectious panel for diseases endemic to Southeast Asia returned negative. A CT abdomen and subsequent PET-CT scan confirmed diffuse lymphadenopathy in bilateral cervical, axillary, external iliac, and abdominal lymph nodes along with increased bone marrow activity. Lymphoma was high on the differential given his clinical picture. However, a bone marrow biopsy revealed no evidence of a neoplastic process.
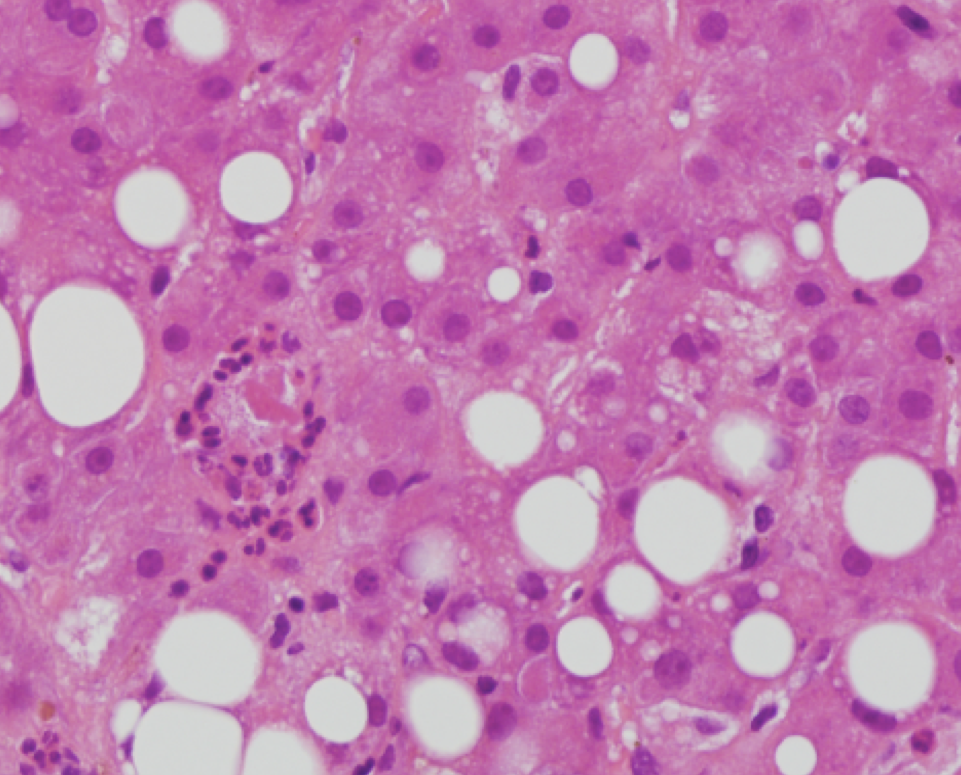
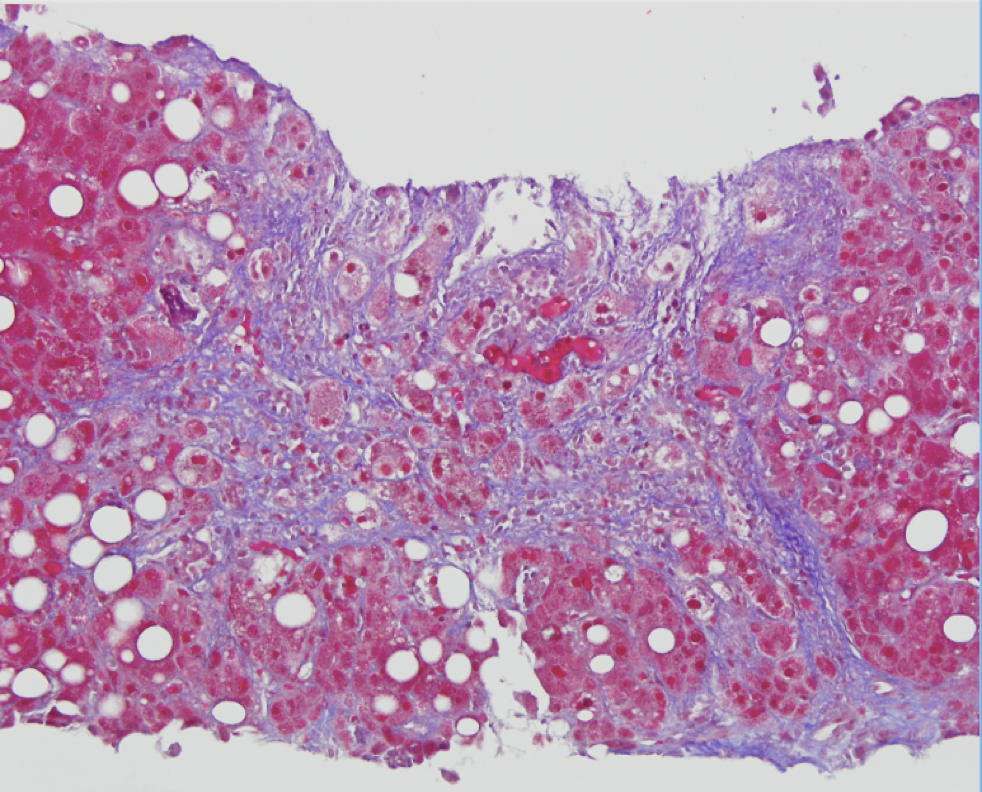
Meanwhile, the patient’s bilirubin continued to rise to 20 mg/dL. Next, a transjugular liver biopsy with pressure measurements was performed with a hepatic venous pressure gradient of 10 mmHg, confirming portal hypertension. Histology showed steatosis, mild portal fibrosis, and Mallory body formation with neutrophilic infiltrates, consistent with a diagnosis of alcoholic hepatitis. He was started on prednisolone and completed a 28-day course of steroids with complete resolution of fevers, ascites, and biochemical abnormalities.
Conclusions: This case is important for hospitalists because it illustrates the importance of considering alcoholic hepatitis as a diagnosis more often, even when the patient’s reported history and findings do not fit the classic presentation. Alcoholic hepatitis has a high mortality rate, so early recognition and intervention can increase patient’s chance for recovery. In this case, even though the presentation was puzzling with generalized lymphadenopathy and clinical symptoms suggestive of an underlying malignancy, by pursuing a liver biopsy the team was able to intervene in a timely manner.