Background: Federally Qualified Health Centers (FQHCs) are community-based primary care centers serving those in medically underserved areas (MUAs) regardless of barriers. Academic Medical Centers (AMCs) are often similarly located and serve as the population health manager for their local communities. AMCs, however, often struggle to deliver care to these communities in a financially sustainable way. We will describe a unique collaboration bringing together an AMC and FQHC in the care of the local community, combining unique resources afforded by the FQHC with the clinical and academic acumen of the AMC.
Purpose: Identify a Johns Hopkins Medicine (JHM) clinic and FQHC partner for transition to a collaborative model aimed at enhancing access to care, advancing efforts to address social determinants, and strengthening the AMC tripartite mission through expanded clinical service offerings, enhanced teaching programs, and community research opportunities.
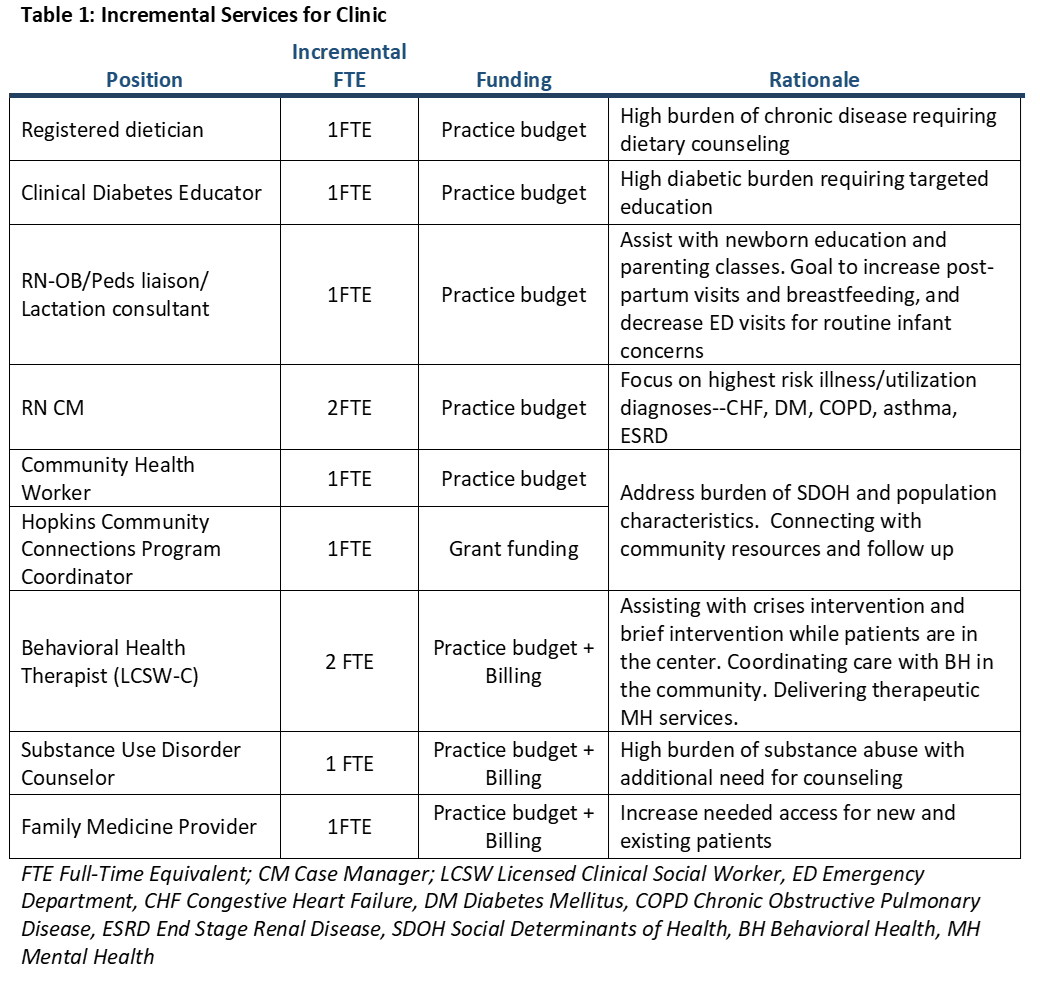
Description: JHM sought to assemble an integrated AMC-FQHC model, leveraging the strengths of each organization to provide financially-sustainable, high-quality care in a MUA. Applications were solicited from local FQHCs for partnership with core agreement to lease providers, share an EMR, and support the education and research mission. An FQHC with a shared mission and well-established priorities was selected. A multidisciplinary group identified incremental roles needed to support the clinic patient population.A large, non-hospital based primary care clinic that included adult and pediatric care, OB/GYN, dental, and pharmacy services located in a MUA was selected for partnership. The site transitioned to an FQHC with the following key elements:• Providers and staff remained employed by JHM, leased to the FQHC for provision of care• FQHC site was hosted on the Hopkins Epic platform• Resident training programs and Hopkins-sponsored research continued at the FQHC• Enhanced access was provided to additional Medicaid MCOS and uninsured patient populations• Eleven incremental roles were approved to enhance key wraparound resources including behavioral health, substance use disorder counseling, community navigation, and nutrition servicesEnhanced revenue from FQHC billing improved the financial position of the clinic. The AMC provided grant funding to support operations and broadened resources. The FQHC received additional grants for COVID initiatives, HIV programing, and behavioral health. The academic missions were maintained providing a unique training environment for primary care residents and a site for community-based research.
Conclusions: Through AMC and FQHC partnership, progress can be made towards the provision of financially sustainable care in underserved areas while preserving the tripartite mission of academic medicine, with considerable pedagogical and research opportunities.The FQHC-AMC collaboration affords a unique approach to care of vulnerable patient populations, marrying expertise in community navigation with access to AMC clinical expertise and academic endeavors. Financially, it brings a viable model for primary care of under and uninsured patient populations and potential financial backing of a large health system, creating much needed stability in the care model. Next steps include tracking outcomes of trainees, furthering research opportunities, and determining best practices for other AMCs following similar strategies.