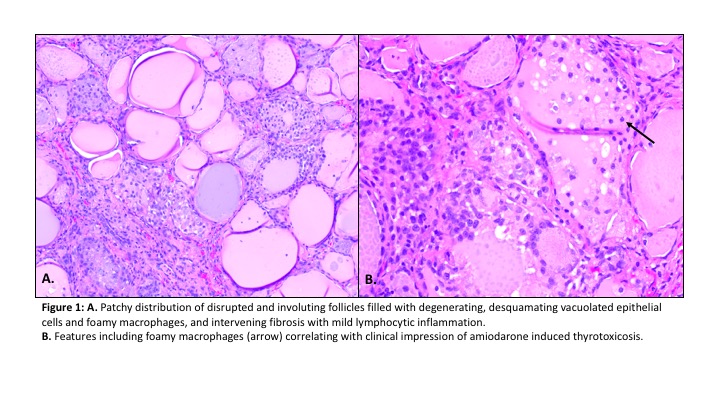
Case Presentation: A 73-year-old female with coronary artery disease, biventricular systolic heart failure requiring implantable cardiac defibrillator (ICD), paroxysmal atrial fibrillation (A-fib) treated with amiodarone for 2 years presented with abdominal pain, nausea, loss of appetite for 1 month. She also reported a recent ICD discharge. Initial vital signs were remarkable for a blood pressure of 215/91. On physical exam she appeared comfortable. She had a nontender thyroid without enlargement or nodules. There was no proptosis. On abdominal exam there was mild diffuse tenderness. Laboratory evaluation revealed elevated troponin at 0.342 ng/mL(<0.04 ng/mL), undetectable TSH, fT4 of 3 ng/dL(0.9-1.7 ng/dL), total T3 of 79 ng/dL(80-200 ng/dL). TPO and TSI antibodies were negative. Thyroid ultrasound showed normal size and echogenicity with few scattered cystic nodules. There was mildly reduced heterogeneous tracer uptake on technetium scan, consistent with thyroiditis. ICD interrogation revealed one episode of ventricular tachycardia and multiple episodes of A-fib with rapid ventricular rate. Electrocardiogram showed no acute changes. The clinical presentation and labs were consistent with amiodarone induced thyrotoxicosis (AIT). She was initiated on prednisone, methimazole, and cholestyramine, in addition to her beta blocker. Despite medical therapy, fT4 continued to uptrend, peaking at >5.2 ng/dL. She underwent plasmapheresis as a bridge to thyroidectomy. After surgery, fT4 normalized, and her abdominal symptoms resolved. Final surgical pathology revealed follicular epithelial degeneration, foamy histiocytes, and mild lymphocytic inflammation, consistent with AIT.
Discussion: AIT is a life-threatening disorder that can present with cardiac arrhythmias or heart failure exacerbation. The prevalence ranges from 2-10%, with fewer cases in Iodine sufficient areas. AIT is due to disruption of thyroid hormone synthesis or direct damage to thyroid cells. Diagnosis is made when TSH is suppressed and fT3, fT4 increased, although in rare cases fT3 can be normal. Type 1 is due to increased synthesis of thyroid hormone and is treated with thionamides or radioablation. Type 2 is caused by increased hormone release from destructive thyroiditis and responds to glucocorticoids. When the type is unclear as in this case, patients are treated as both. AIT can occur at almost any time during amiodarone therapy. Signs and symptoms range from asymptomatic presentation discovered on routine labs to typical hyperthyroid symptoms such as palpitations and heat intolerance. Classic symptoms of thyrotoxicosis may be absent due to antiadrenergic action of amiodarone and its impairment of conversion of T4 to T3. Besides the arrhythmia, her symptoms of abdominal pain and nausea were atypical. In cases like this, surgery is indicated if medical therapy is unsuccessful. Plasmapheresis can remove cytokines, antibodies and thyroid hormones from plasma, resulting in improvement in thyrotoxicosis within 3 days, however it is a temporizing measure. There is no immediate benefit to discontinuing amiodarone given the long half-life.
Conclusions: The hospitalist role of taking a comprehensive medical history including medication reconciliation is of utmost importance. The question of whether a certain drug is causing the patient’s presenting symptoms can be difficult to tease out. This case serves as a reminder to keep medication side effects on the differential.