Background:
The Modified Early Warning System (MEWS) is a validated tool that aids in the identification of hospitalized patients at risk for clinical deterioration. With rapid response team involvement, the MEWS has demonstrated reduced in‐hospital mortality in the United Kingdom1, and the Royal College of Physicians has encouraged adoption of a standardized version at all hospitals across England. The majority of early warning systems reported in the literature utilize manual tabulation and reporting, a time‐consuming process prone to error.
Purpose:
Our goal was to utilize the electronic health information system (EHIS) to implement an automated version of the MEWS on all medical and surgical units at Providence St. Vincent Medical Center in Portland, Oregon. We hypothesized that automated earlier identification of patients at risk for clinical deterioration along with a standardized response protocol would improve patient safety in the hospital.
Description:
The automated MEWS, which is calculated any time a patient’s vital signs are measured, incorporates four vital signs (temperature, heart rate, blood pressure, and respiratory rate) and scores each individually before combining them into an aggregate score, the MEWS score. Each time the MEWS score equals or exceeds four, the EHIS automatically triggers a paging system to alert the appropriate charge nurse for the patient. These pages, which read “MEWS alert,” display the MEWS score and contributing vital signs. The charge nurse then initiates a standardized nursing workflow via the direct care nurse, who repeats the vital signs and urgently notifies the attending physician. If the score meets or exceeds five, an automated page is also sent to the lead rapid response team nurse in the ICU, who responds to the bedside. After implementing the automated MEWS, a before‐and‐after comparative analysis of inpatient mortality was performed. Mortality rate was defined as percentage of patients with one or more days on a MEWS unit who expired during their hospitalization. Analysis was completed using Chi‐square statistics. The presence of trend was assessed using Cochran‐Armitage statistics. The secular trend bias was investigated using severity‐adjusted expected mortality. A p value of < 0.05 was regarded as being significant. Analysis was performed with SAS 9.3 statistical software (SAS Institute, Cary NC).
Conclusions:
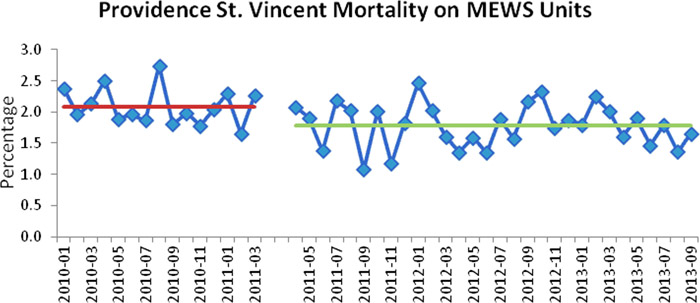
Patients admitted to MEWS units after activation of an automated early warning system had a lower mortality rate than those admitted to the same units prior to MEWS activation, from 2.09% to 1.78% (p = 0.005, Fig. 1). The overall downward trend in mortality was also statistically significant (p = 0.017). Severity‐adjusted expected mortality did not change over time.
1. Moon A et al. An eight year audit before and after the introduction of modified early warning score charts, of patients admitted to a tertiary referral intensive care unit after CPR. Resuscitation 2011;82:150