Background: Late afternoon hospital discharges contribute to admission delays, leading to occupancy increase and increased length of stay. However, prominent workplace barriers often exist towards improvement initiatives that target early discharge. Team members cite timing of rounds, absence of early discharge support resources, communication breakdowns, and increased daytime admission volume as barriers to change. Furthermore, interventions incentivizing early discharges often do not yield sustainable change. Our academic medical center set out to develop a multifaceted, interdisciplinary, systematic approach to improving the discharge process on physician-assistant (PA) staffed Solid Tumor Oncology (STO) services.
Purpose: To streamline the discharge process and to decrease the discharge time on PA-staffed Solid Tumor Oncology services through the implementation of an interdisciplinary structured discharge tool.
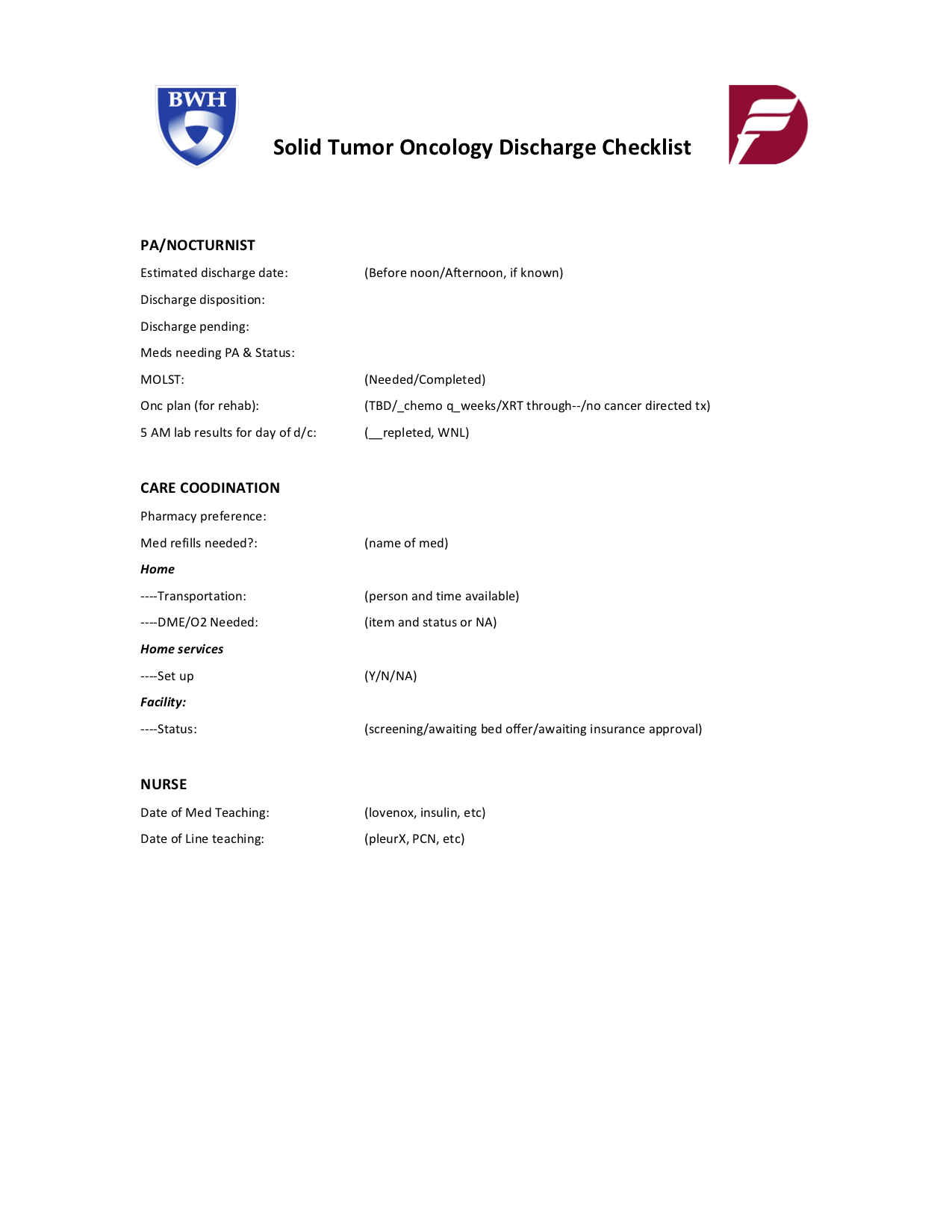
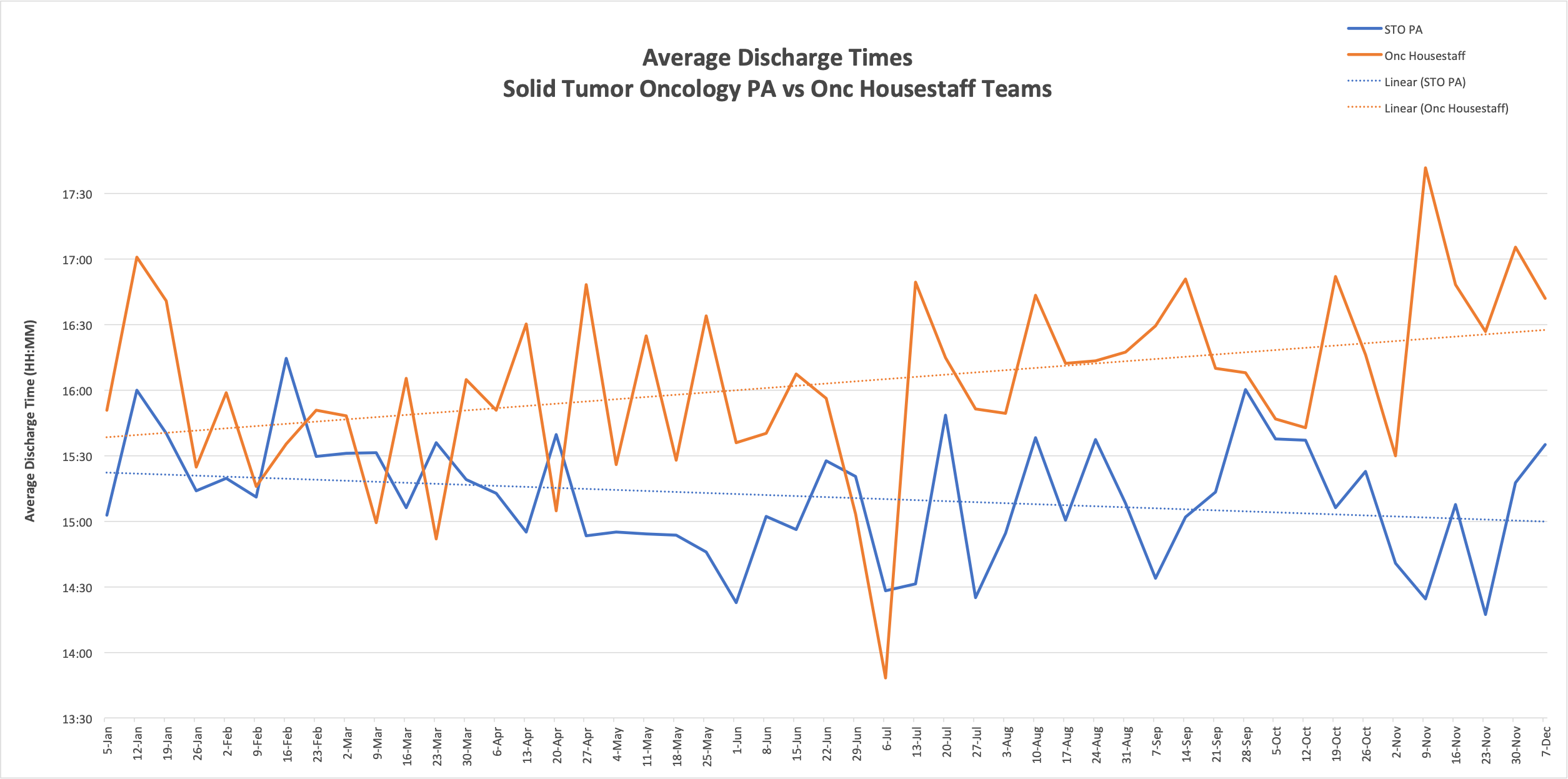
Description: We engaged a group of key stakeholders in the discharge process on PA-staffed Oncology services at BWH, including physician assistants, oncologists, nocturnists, case managers, nurses, and hospital leadership. Most frequent contributing factors to late afternoon discharges were identified: top barriers to early discharge included lack of physician assistant staff support to complete early discharges during rounds and inefficient communication between team members. We focused on creating a “bottom-up,” homegrown, and service-specific innovation that focused on enhancing communication between frontline interdisciplinary team members regarding readiness for discharge and barriers to discharge. Interventions included: identification of early discharges via a daily status email, communications to confirm tasks lists for discharge, and an EMR-based checklist highlighting key tasks in each patient’s discharge process (Figure 1). Nocturnists were utilized to provide late afternoon admission support and follow up on key tasks the evening before discharge. Team members were educated on the checklist during the intervention. Historical data was notable for an average discharge time of 15:45 on STO PA services prior to the intervention. Intervention implementation occurred over a 6-month time period, and data on average discharge times was collected weekly over a 12-month time period and compared to other service lines (Figure 2). During implementation, we saw consistent reduction in discharge time compared prior historical data and to other service lines. Average discharge time was reduced from 15:45 to an average time of 15:07 during the intervention. In the 3-month follow up post implementation, average discharge time remained stable.
Conclusions: Our interventions collectively decreased discharge time by an average of 38 minutes, and we have found that time of discharge has stabilized post-project completion, while the average time of discharge has increased across other service lines. Based on informal feedback from our stakeholders, the most successful components of our intervention included redesigning roles to streamline the discharge process, early discharge support, and enhanced communication in discharge planning. We anticipate that these improvements will lead to increased frequency of discharges before noon and may improve patient outcomes in the discharge process. We plan to disseminate our tool to other services across our hospital.