Background: Improving a patient’s experience with the health care system improves outcomes of care. Glickman et al found that higher patient satisfaction is associated with improved adherence and lower inpatient mortality rates. Boulding et al found that higher patient satisfaction was associated with lower 30- day readmission rates for patients with heart failure, acute MI and pneumonia. While Davidson et al’s 2017 systematic review found a need for more research on interventions that improve patient experience, little is known about interventions that improve experience with hospital medicine physicians. Accordingly, our hospital medicine service formed an internal patient experience committee in the spring of 2018 with the goal of improving our patients’ experience with our physicians.
Methods: Our patient experience committee developed a multi-pronged approach including (1) the establishment of the “Heart of Gold” award to recognize high performers (2) the dissemination of positive patient comments and (3) the implementation of patient centered communication strategies. Patient comments for each quarter along with quantitative scoring were aggregated and analyzed for top performers who were awarded the Heart of Gold. The recognition was announced in our e-newsletter and the recipient received a certificate signed by division chief and chair of the patient experience committee at our monthly team meeting. Positive patient comments were displayed in work rooms, disseminated in our weekly e-newsletter and directly to each physician. Patient centered communication strategies and skill development included strategies such as how to enter the room – initiating and maintaining a respectful etiquette, committing to sit, promoting team members, and unified messaging. We also disseminated tactics on connecting with patients on a personal level to improve alignment of care plans with our patients’ values and motivations.We conducted a retrospective pre-post analysis of Press Ganey (PG) patient experience scores for physicians in the UTSW Division of Hospital Medicine at Parkland Hospital, comparing July 1, 2017 to June 30, 2018 with July 1, 2018 to June 30, 2019. Wilcoxon Rank Sum tests were used to compare median PG scores. A p-value of <0.05 was considered significant.
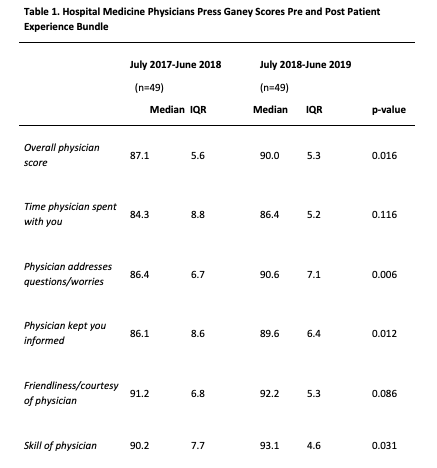
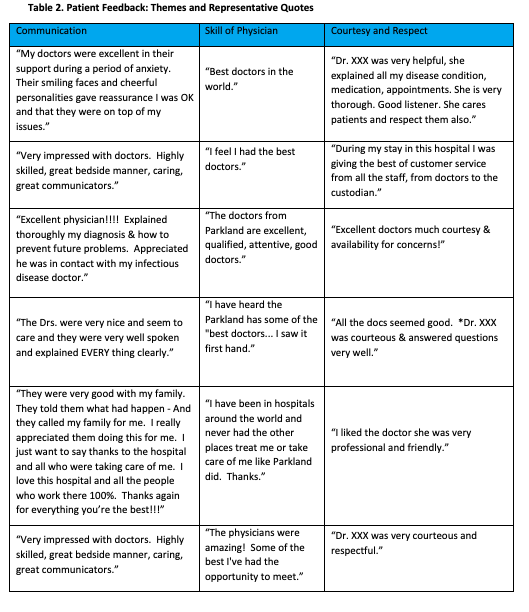
Results: Our overall physician score improved from a median of 87.1 (5.6 IQR) to 90.0 (5.3 IQR) (p = 0.0163) (Table 1). When compared to 300+ bed public hospitals, this correlated to an increase in percentile ranking from close to the 40th percentile to nearly the 75th percentile. While patients did not perceive a change in the amount of time their physicians spent with them (p=0.116), they felt their physicians better addressed their questions and concerns (p=0.006), better kept them informed (p=0.012) and were more skilled (p=0.031).Themes and representative quotes from patient comments are found in Table 2.
Conclusions: Our patient experience committee developed and implemented a grass roots, bundled intervention which improved our patients’ experience with their hospital medicine physicians. Through recognition of high performance, the dissemination of positive comments and the development and dissemination of communication strategies, our patients experienced unprecedented levels of satisfaction with our physicians. Future directions will encompass the sustainment of gains, continuing to refine communication strategies and developing a remediation program for struggling physicians.