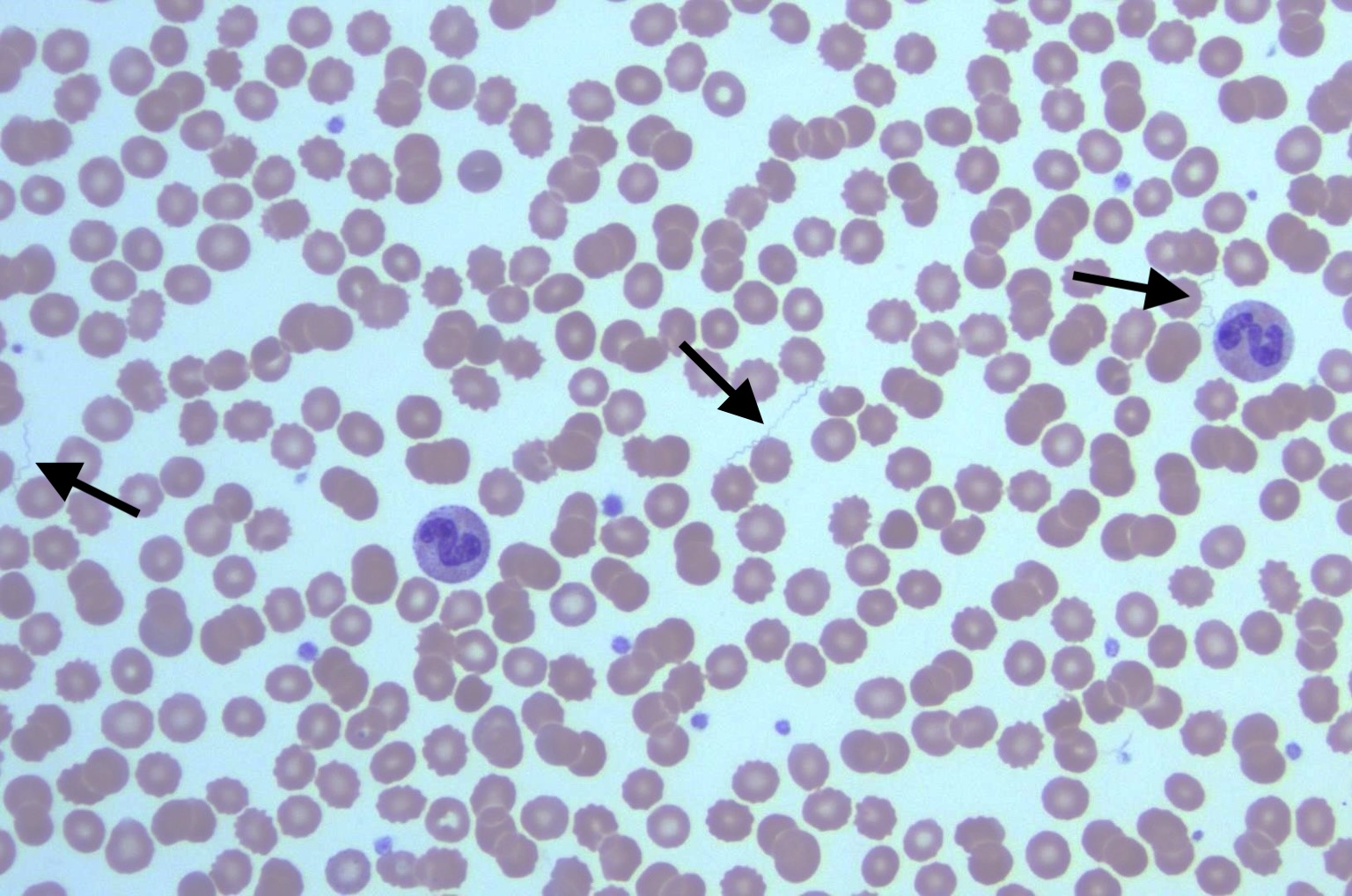
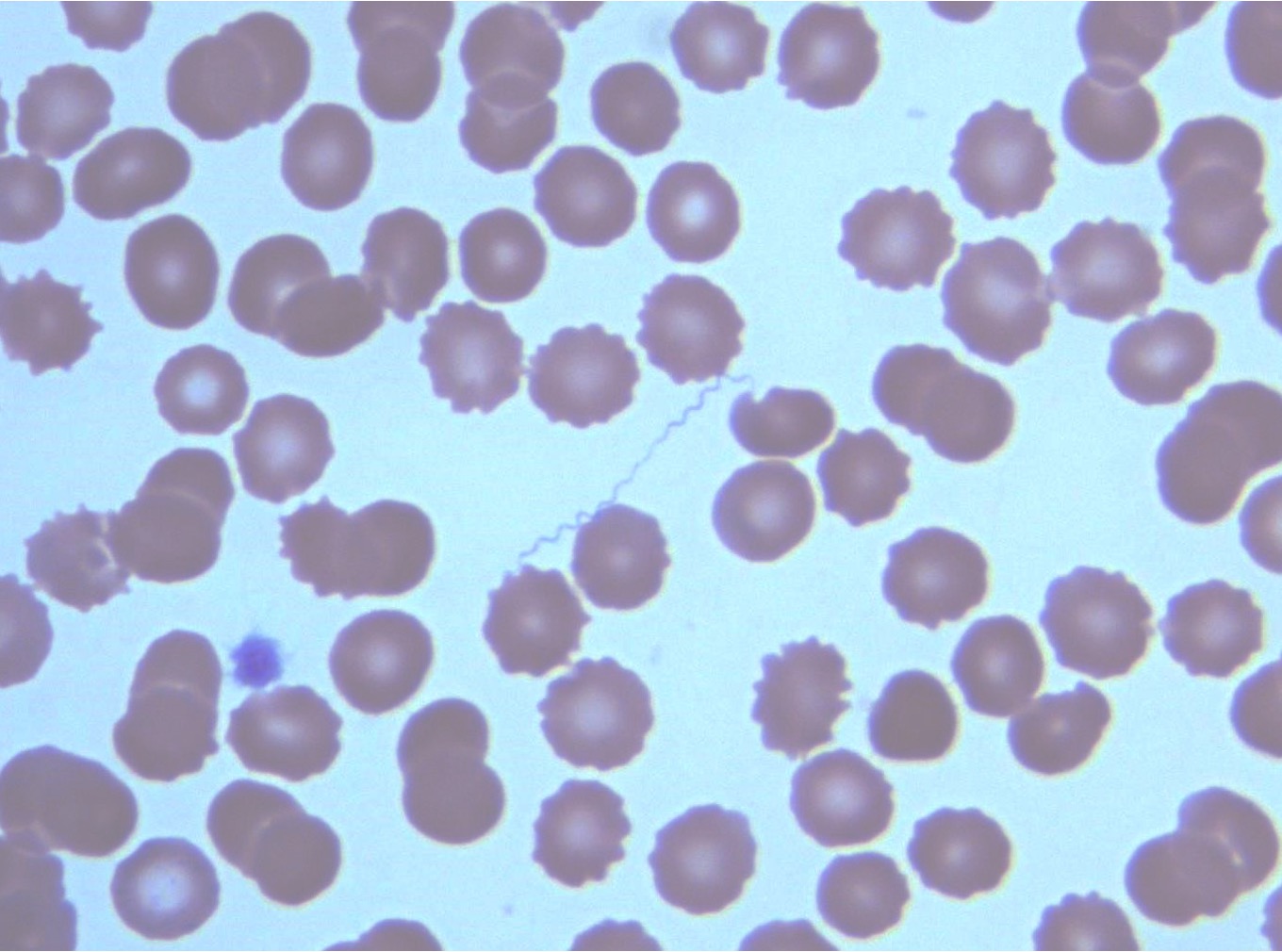
Case Presentation: A 65-year-old woman with a history of migraines without aura and mild asthma presented to a Wisconsin emergency department with a two-day history of fevers and altered mental status following a five-week stay in Colorado. Symptoms included subjective fevers and urinary incontinence in addition to neurological concerns such as confusion, forgetfulness, and difficulty completing tasks. She also reported multiple insect bites of an unclear source. Initial exam was notable for a temperature of 38.8°C and a small, erythematous lesion on her right thigh. Laboratory findings included elevated transaminases (AST 106 U/L, ALT 116 U/L), hyperbilirubinemia (total bilirubin 2.1 mg/dL) thrombocytopenia (103 K/µL), mild hyponatremia (132 mM/L), mild hypokalemia (3.1 mM/L), and elevated procalcitonin (2.26 ng/mL). Empiric cefepime and vancomycin were started, and the patient was admitted to the inpatient general medicine service. The patient clinically worsened overnight, with tachycardia and hypotension refractory to fluids. Doxycycline was empirically added given the high concern for tick-associated pathology. A peripheral blood smear revealed spirochetes, leading to a presumptive diagnosis of Tick-Borne Relapsing Fever (TBRF). The patient was then transitioned to ceftriaxone and doxycycline, and her neurological status improved rapidly with antibiotics. After one night in the hospital, she was discharged with a 10-day course of oral doxycycline. At discharge, abnormal liver function tests and thrombocytopenia had improved. A primary care follow-up visit a few days later showed a near-complete resolution of symptoms and normalization of labs. Relapsing fever Borrelia species PCR was positive 5 days after her presentation, confirming the diagnosis.
Discussion: TBRF is a zoonotic infection caused by the Borrelia genus of spirochetes, primarily in southwestern United States [1]. With the rise in tick-borne illnesses worldwide due to climate change [2], this case of TBRF in Wisconsin highlights the importance of considering this diagnosis in non-endemic areas. TBRF often presents with non-specific symptoms like relapsing fever (nearly 100% of cases) [3], headaches (63%), myalgias (59%), chills (54%), and nausea/vomiting (45%) and can manifest as severe sepsis requiring hospitalization [1,4]. Neurological involvement is likely secondary to systemic effects of spirochetemia rather than direct CNS invasion [3]. Risk factors include recent travel to the southwestern United States, the presence of ticks, and cabin exposure [1,3]. Peripheral blood smear during febrile episodes can provide a rapid diagnosis. PCR is more sensitive but is expensive and has a long turnaround time [3].
Conclusions: Consider tick-borne disease in patients with unexplained fever, thrombocytopenia, and/or elevated transaminases. High suspicion for tick-related illnesses may warrant empiric treatment with doxycycline. Early consideration of TBRF, even in non-endemic regions, is essential for prompt diagnosis and treatment.