Case Presentation:
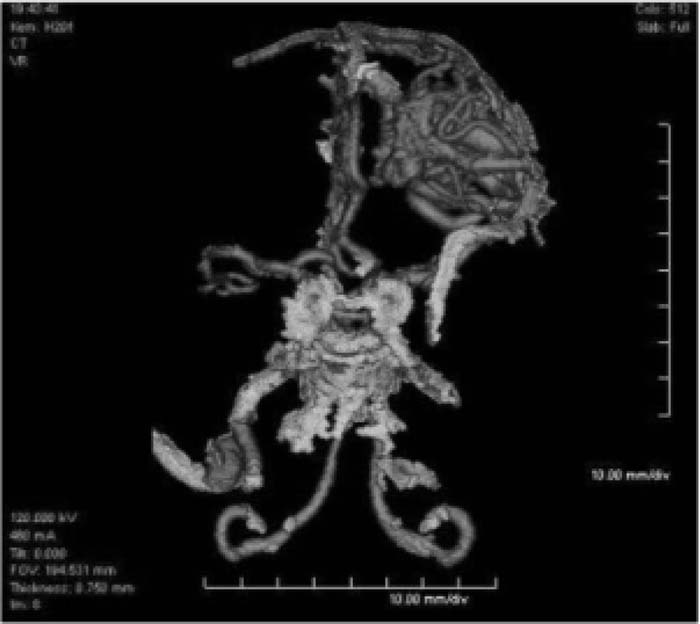
A 43‐year‐old female with a history of epilepsy presented after a witnessed seizure. The patient had been seizure free for more than 15 years and had been taking her medications as prescribed. In the emergency room, the patient experienced 2 generalized tonic clonic seizures, which were treated with lorazepam and fosphenytoin. She denied other past medical history but has multiple family members with seizure disorder. Her medications included carbamazepine and divalproex sodium. Review of systems was unremarkable. On physical exam the patient was slightly somnolent but alert, oriented, and otherwise neurologically intact with stable vital signs. CBC, electrolytes, urinary drug screen and urinalysis were unremarkable. TTie patient had a slightly decreased valproic acid level at 43.1 μg/mL (normal range 50‐100 μ/ml) and a normal carbamazepine level. Standard head computed tomography (CT) and subsequent CT angiogram of the brain demonstrated a large, left frontal AVM measuring 3.7 × 3.3 cm without evidence of intracranial hemorrhage. The patient stated she had never had neuroimaging prior to this incident. After medication titration, she was evaluated by neurosurgery and the decision was made to proceed with outpatient Cyberknife treatment.
Discussion:
Arteriovenous malformations (AVMs) in the central nervous system are the most dangerous congenital vascular malformation, and their management is of significance as complications arising from these lesions cause substantial morbidity and mortality. Large AVM generally present with intracranial hemorrhage or seizures in patients who otherwise have no history of such. At The same time, a history of epilepsy does not exclude the need for imaging in a patient with a seizure. In our case, an appropriately ordered CT scan discovered a large cerebral AVM which likely induced the epileptic event. After discovery of the lesion, definitive diagnosis is best achieved by angiography, which allows determination of size and angioarchitecture and is imperative to guide further therapeutic interventions. MRI is useful to locate remote bleeding sites and follow patient treatment. Hemorrhage, which carries a known incidence/year based on size, is the most dreaded complication of AVM, and treatment is aimed at avoiding these events.
Conclusions:
Although resources should be used with discretion, a new seizure warrants brain imaging, especially if the patient has otherwise been well. Historically, therapeutic interventions for asymptomatic AVM display no clear benefit; however, treatment is clearly warranted in the above case.
Author Disclosure:
K. Khosa, none; G. Kuchmak, none; R. Wardrop, none.