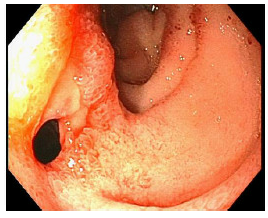
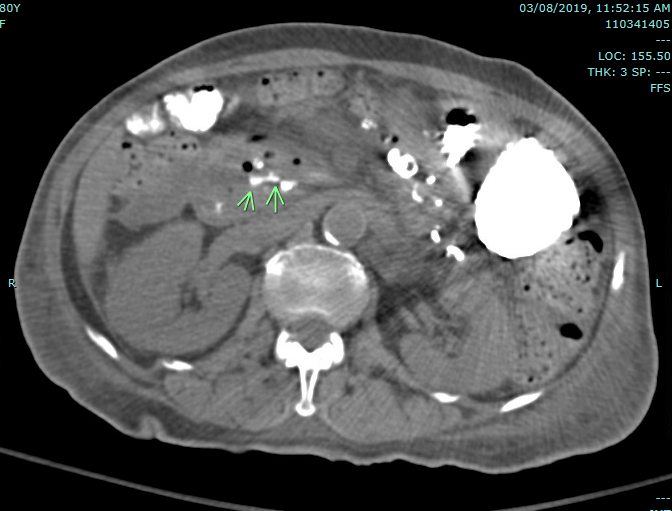
Case Presentation: An 80 year-old female presented to the emergency room with shortness of breath and melena. She was afebrile, with blood pressure of 121/70 and heart rate 93. Labs showed hemoglobin of 5.2 g/dL with normal INR and platelet count. She underwent an upper endoscopy revealing a 2 mm clean-based duodenal ulcer. As this did not account for her melena, she underwent a colonoscopy as well as video capsule endoscopy which did not show any clear source of bleeding. As she continued having a drop in her hemoglobin and melena, a CT was performed revealing draining biliary contrast from the second and third portion of the duodenum, concerning for bleeding as well as signs of chronic pancreatitis. A second EGD was performed which revealed a duodenal mucosal defect suspicious for a fistulous opening into the pancreas with evidence of active bleeding. A repeat CT revealed extraluminal contrast extravasation in the retroperitoneum medial to the second part of the duodenum and close in proximity to the superior mesenteric vein. She was taken to interventional radiology where angiography did not reveal active extravasation, so empiric embolization of the gastroduodenal artery was performed. Magnetic resonance imaging of the abdomen showed findings consistent with chronic pancreatitis with dilation of the main pancreatic duct and 1 mm pseudocysts in the body and tail. Her melena resolved and her hemoglobin stabilized prior to discharge.
Discussion: Pancreatic fistulas result from disruption of the pancreatic duct such as in pancreatic resection, trauma, as well as acute and chronic pancreatitis. Non-iatrogenic pancreatic fistulas can be asymptomatic or symptomatic, manifesting as gastrointestinal bleeding in rare circumstances. Bleeding from pancreatitis is a rare complication and occurs 10-15% of patients with chronic pancreatitis and 6-30% with pancreatic pseudocysts. Pancreatic structures can be destroyed by enzyme digestion and necrosis. This may create pseudoaneurysms which may create cavities, fistulous tracts, or rupture if they involve arterial or venous vasculature. The splenic and gastroduodenal artery are the most commonly affected. The clinical presentation may vary depending on location and severity of bleeding from asymptomatic anemia to hypovolemic shock. Diagnosis involves abdominal CT and upper GI endoscopy, however laparotomy sometimes may make the only accurate diagnosis. Therapeutic approach can be achieved by embolization or surgery. In our case, bleeding may have resulted from spontaneous hemorrhage into the cystic cavity or as a result of erosion in the superior mesenteric vein given the proximity of the SMV on imaging. This case highlights the need to maintain a high clinical suspicion for pancreaticoduodenal fistulas in patients with a history of pancreatic disease presenting with GI bleeding.
Conclusions: Pancreatic fistulas have been described in the setting of pancreatic resection, trauma, and less commonly in patients with acute or chronic pancreatitis. Spontaneous pancreatic fistulas resulting in gastrointestinal bleeding are rare. Her case highlights the importance of appropriate imaging and a multi-specialty team in diagnosis and therapy of a rare bleeding pancreaticoduodenal fistula.