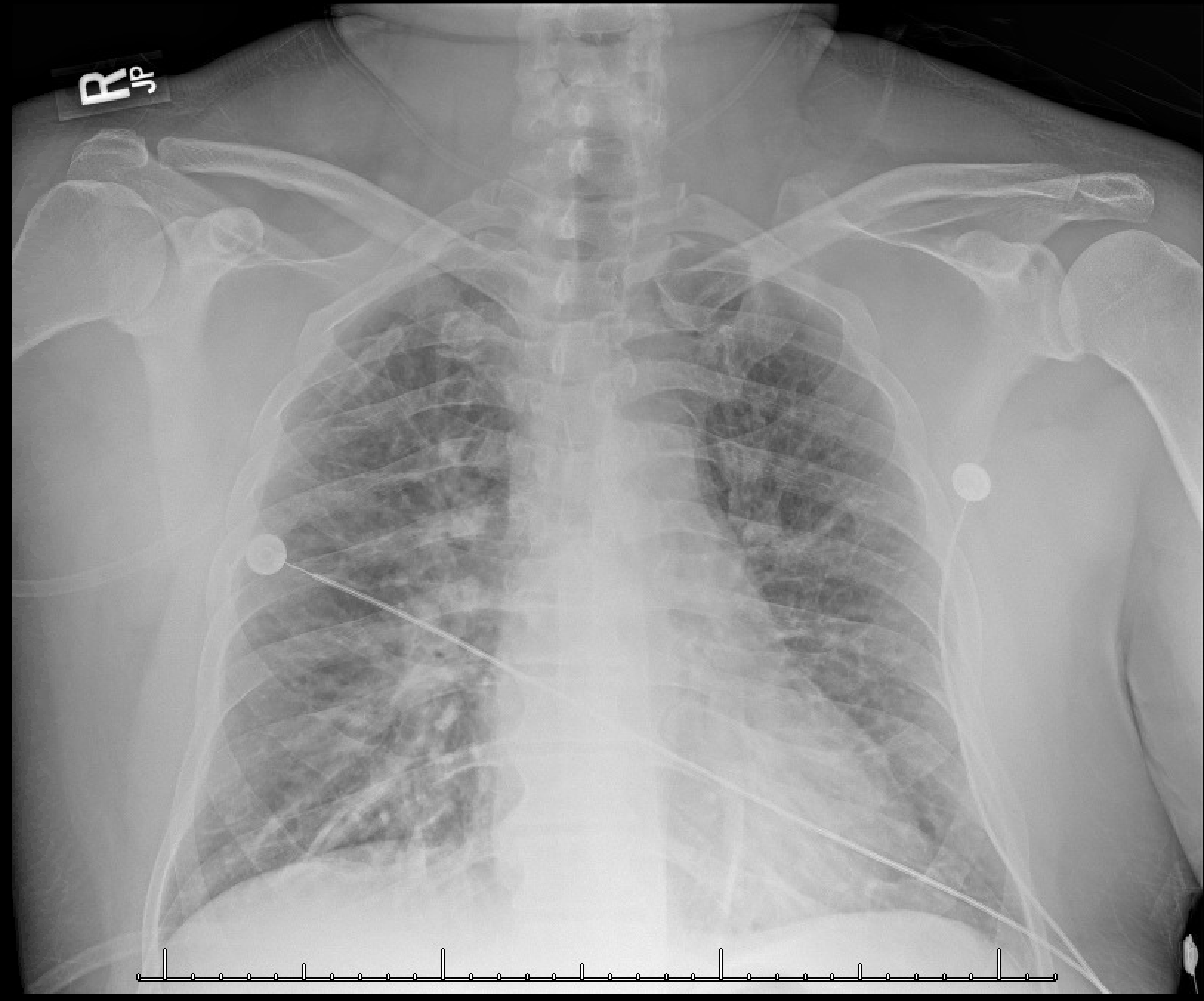
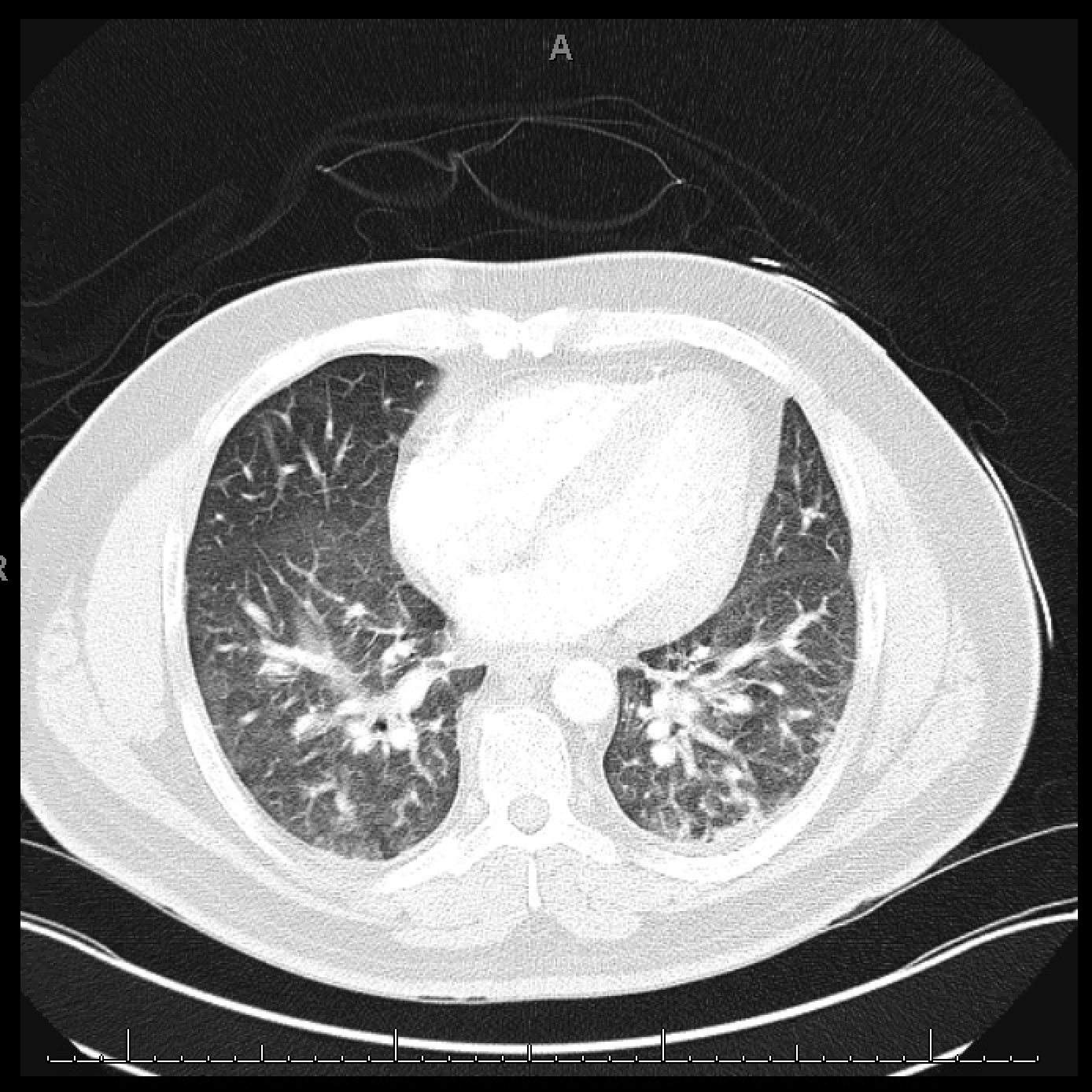
Case Presentation: 47-year-old male with past medical history of fibromyalgia, hypertension, and mild asthma presented with shortness of breath during a double red cell donation (DRCD). DRCD is a procedure where two packs of whole blood are taken from a donor, and plasma is separated from them, this plasma is then transfused back to the donor. During the post-donation plasma infusion, the patient developed sharp pain in his ears, shortness of breath, and a metallic taste in his mouth. His symptoms progressed to chest pain, dizziness, shortness of breath, pallor, shivers, numbness and tingling in his extremities. He had undergone this same procedure 6 times in the past, the last being 6 months prior to presentation, without any complications. On presentation: Vital signs: temp 38.9C, pulse 102, resp 18/min, BP 79/41, oxygen saturation 83%. Pulmonary and cardiovascular exam was significant for respiratory distress, rales in all lung fields, and no pedal edema. Labs were significant for potassium 2.9, troponin 0.037 (elevated), proBNP 38.1 (normal), d-dimer 11,268 (elevated). Hemoglobin, platelet count and INR were normal. A direct coombs test, LDH, haptoglobin, fibrinogen were all negative. EKG showed sinus tachycardia, no ST elevation. CT angiography chest showed bilateral pulmonary edema, but absence of pulmonary emboli or infiltrates. Extensive work up including Streptococcal pneumonia antigen, Legionella urinary antigen, respiratory viral panel, blood cultures were all negative. Echocardiogram was done to rule out a cardiac etiology of pulmonary edema and showed an LVEF of 60%. Chest examination suggested resolution of pulmonary edema on day 2 of admission. Empiric treatment was given for pneumonia, he was discharged with outpatient follow-up.
Discussion: The diagnosis of TRALI (transfusion associated acute lung injury) is based on clinical and radiographic findings. It should be suspected when a patient develops acute respiratory distress within 6 hours of a transfusion in the absence of left atrial hypertension or circulatory overload. A normal BNP and echocardiogram ruled out transfusion associated circulatory overload in our patient. Literature regarding developing TRALI after receiving one’s own plasma back after a red cell donation is sparse, which made our case challenging. Considering that TRALI is mostly an immune-mediated reaction to donor cells, our case signifies there might be a process similar to TRALI from self-sensitization to plasma cells during the cell separation and transfusion process of DRCD.
Conclusions: In summary our case signifies that there is potential for a process similar to TRALI while the donor is receiving his own plasma back during a double red cell transfusion. The sparsity of literature on the subject makes the diagnostic evaluation and treatment largely up to the treating physician and further investigation is required to look into how diluents and tubing of the intravenous lines can potentially lead to self-sensitization.