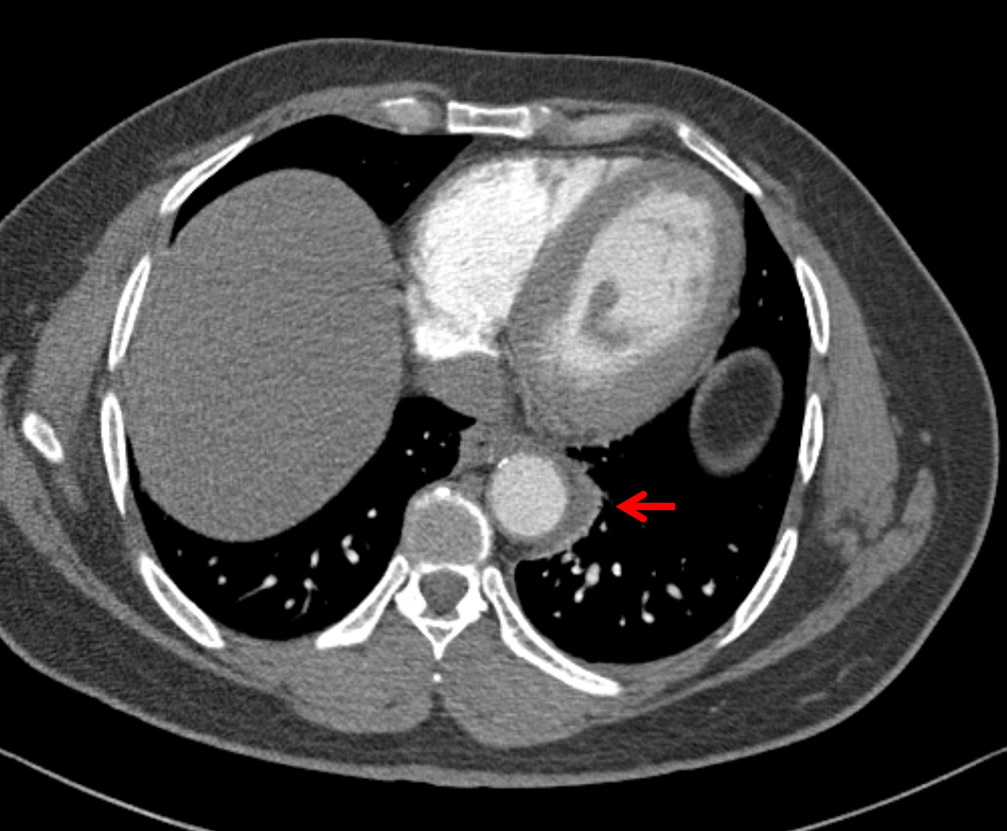
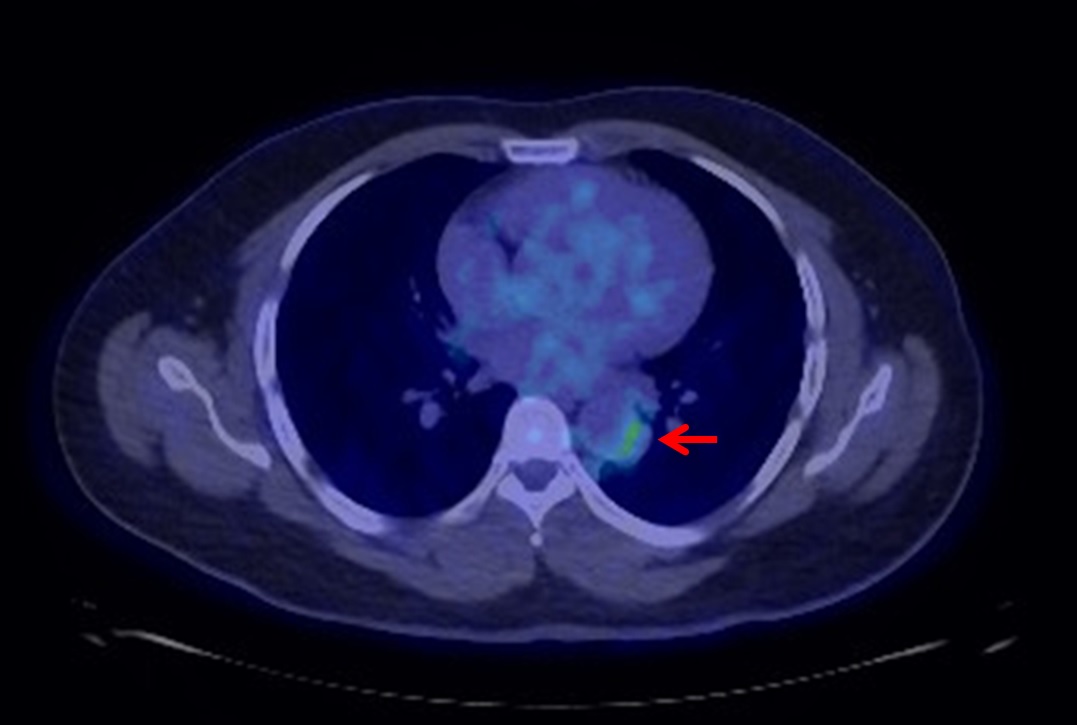
Case Presentation: A 38-year-old African male with no medical history presented to the emergency department with chronic, intermittent epigastric abdominal pain. Physical exam revealed a diminished left radial pulse but was otherwise unremarkable. Labs were notable for an elevated C-reactive protein (CRP) to 23.7 mg/L (normal <8) and positive QuantiFERON consistent with latent tuberculosis (TB). CT abdomen and pelvis revealed diffuse abdominal lymphadenopathy. CT-guided biopsy of an enlarged node demonstrated adipose tissue with chronic inflammation. Bacterial, fungal, and mycobacterial cultures were negative.Several weeks later, the patient developed pleuritic chest pain and was admitted to the internal medicine service. CT chest angiography showed perivascular inflammation involving the thoracic aortic arch, supra-aortic vessels, and descending thoracic aorta concerning for active large vessel vasculitis (figure 1). CT abdomen and pelvis showed occlusion of the celiac artery with superior mesenteric artery (SMA) stenosis, and large collaterals between the SMA and inferior mesenteric artery. Ultrasound of the lower extremities revealed chronic occlusion of the right superficial femoral artery.The distribution of this patient’s vasculitis was most consistent with Takayasu arteritis (TA), despite his uncommon demographic. On further questioning, the patient reported chronic lack of pulse in the left arm with previous symptoms of claudication in the left arm and right leg when he was a teenager. Based on this history and imaging, this was thought to be a chronic process that had been progressing for at least twenty years. PET-CT showed mild FDG uptake throughout the thoracic aorta, leading to speculation that this was only mildly active disease that did not require urgent immunosuppressive therapy (figure 2). The patient was treated for latent tuberculosis prior to initiating treatment for TA.
Discussion: TA is a large-vessel vasculitis that preferentially involves the ascending aorta and aortic arch. It is most common among Asian females, with a peak age of onset between twenty to thirty years. The clinical presentation is highly variable, making it challenging to recognize and diagnose. Patients typically present with nonspecific constitutional symptoms including fevers, weight loss, and generalized malaise. Patients eventually develop stenotic vessels, leading to decreased pulses, asymmetric blood pressures, and claudication symptoms. TA can similarly involve lymph nodes and lead to diffuse lymphadenopathy. Treatment consists of immunosuppressive therapy, which was contraindicated in our patient with latent TB. Acute phase reactants, including CRP, do not correlate well with disease activity. However, the degree of FDG uptake during PET-CT correlates with future clinical relapse and is useful in the prognostic work-up of TA.
Conclusions: We report an unusual case of widespread TA in a 38-year-old African male presenting with chronic abdominal pain. He had vasculitis spreading from the thoracic ascending aorta to the femoral artery with diffuse abdominal lymphadenopathy. Despite having stenosis within several vessels, he developed extensive collaterals and had no claudication symptoms at the time of presentation. We hypothesize that the delay in diagnosis and lack of treatment for nearly twenty years led to this extreme level of vascular involvement. This case further highlights the utility of PET-CTs in the prognostic work-up of large-vessel vasculitis.