Background: Research suggests that COPD patients with low peak inspiratory flow rate (PIFR, <60 L/min) may have poor bronchodilation resulting from ineffective inhalation of medication using dry powder inhalers (DPI). This study evaluates the real-world treatment patterns among COPD patients admitted for an exacerbation and have low PIFR at the time of discharge.
Methods: Data from the first 111 patients enrolled in a prospective observational study at 7 US sites were used in this analysis. Patients were enrolled at hospital discharge following treatment for a COPD exacerbation. PIFR was measured using the InCheckTM DIAL to simulate resistance of the Diskus® DPI. Patients were classified into low PIFR (<60 L/min) or normal PIFR (≥60 L/min) cohorts. Prevalence of low PIFR was calculated from all available patients, including patients who were later screened out (n=11) to achieve equal cohort sizes. COPD treatments before, during and after hospitalization, baseline demographics, clinical characteristics, and COPD-related health status were collected for the 100 patients who were enrolled and followed up. Differences between the low and normal PIFR cohorts were tested by independent sample t-tests for continuous outcomes, and using chi-squared tests for categorical measures.
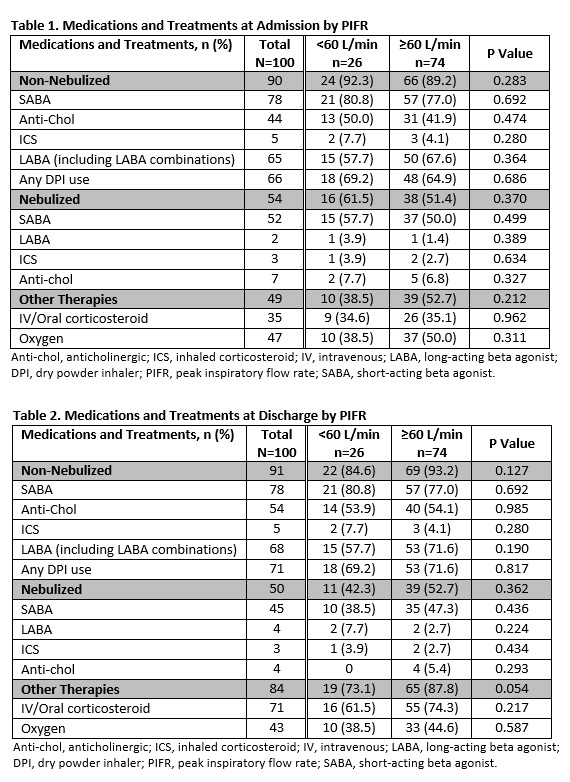
Results: Mean PIFR was 73.7±22.84 L/min. Low PIFR was observed in 23.4% (26/111) of patients. In patients included for baseline analysis and follow-up (n=100), the mean age was 63.2±9.82 years and 41% were female. The use of DPIs at admission (69.2% vs 64.9%, P=0.686; Table 1) during hospitalization (53.9% vs 62.2%, P=0.457) and at discharge (69.2% vs 71.6%, P=0.817; Table 2) were similar among the low and normal PIFR cohorts, respectively. Overall, treatments at discharge were similar to those at admission, with the exception of increased intravenous/oral corticosteroid use at discharge in both cohorts (low PIFR: 34.6% vs 61.5%, P=0.0196; normal PIFR: 35.1% vs 74.3%, P<0.0001) and increased inhaled anticholinergic use at discharge in the normal PIFR cohort (41.9% vs 54.1%, P=0.029). There was a trend towards decreased use of nebulized treatments between admission and discharge in the low PIFR cohort (61.5% vs 42.3%, P=0.0588).
Conclusions: In this interim analyses, approximately one-fourth of COPD patients had a PIFR <60 L/min at the time of discharge for a COPD exacerbation. Treatment patterns were similar for the low and normal PIFR cohorts at admission and discharge. Despite the potential for ineffective inhalation of their medications with DPI usage, nearly 70% of patients in the low PIFR cohort received medications as a DPI. Nebulized medications can serve as appropriate alternative treatments for patients with low PIFR but these treatments are underutilized.