Background: Readmission among Inflammatory Bowel Disease (IBD) inpatients is common, as is opioid use. Opioid use for IBD has been associated with an increased risk of infection and death, but inconsistently with readmissions. Increasingly, cannabis is viewed as a potentially safer alternative to opioids, though with limited study of potential adverse outcomes such as hospital readmissions. Our aim was to examine cannabis use and the risk of 30 and 90-day hospital readmission.
Methods: We conducted a retrospective review of all adult patients admitted for an IBD exacerbation from 01/01/2016 to 03/01/ 2020 within the Northwell Health Care system. Patients were identified by either a primary or secondary ICD10 code (K50.xx, K51.xx, K52.3), limited to those with an IBD exacerbation defined by use of IV solumedrol and/or biologic therapy. Pregnant patients and those with IBD related surgeries were excluded. A natural language search of admission documents was performed for the terms “marijuana”, “cannabis”, “pot” and “CBD”. Manual chart review was then performed to confirm cannabis use. IBD disease type, age, gender, race, Charlson comorbidity index (CCI), inpatient opioid use, length of stay (LOS) were defined. Logistic regression modeling examined the association between cannabis and readmissions. Analysis was limited to the first/index admission for each patient.
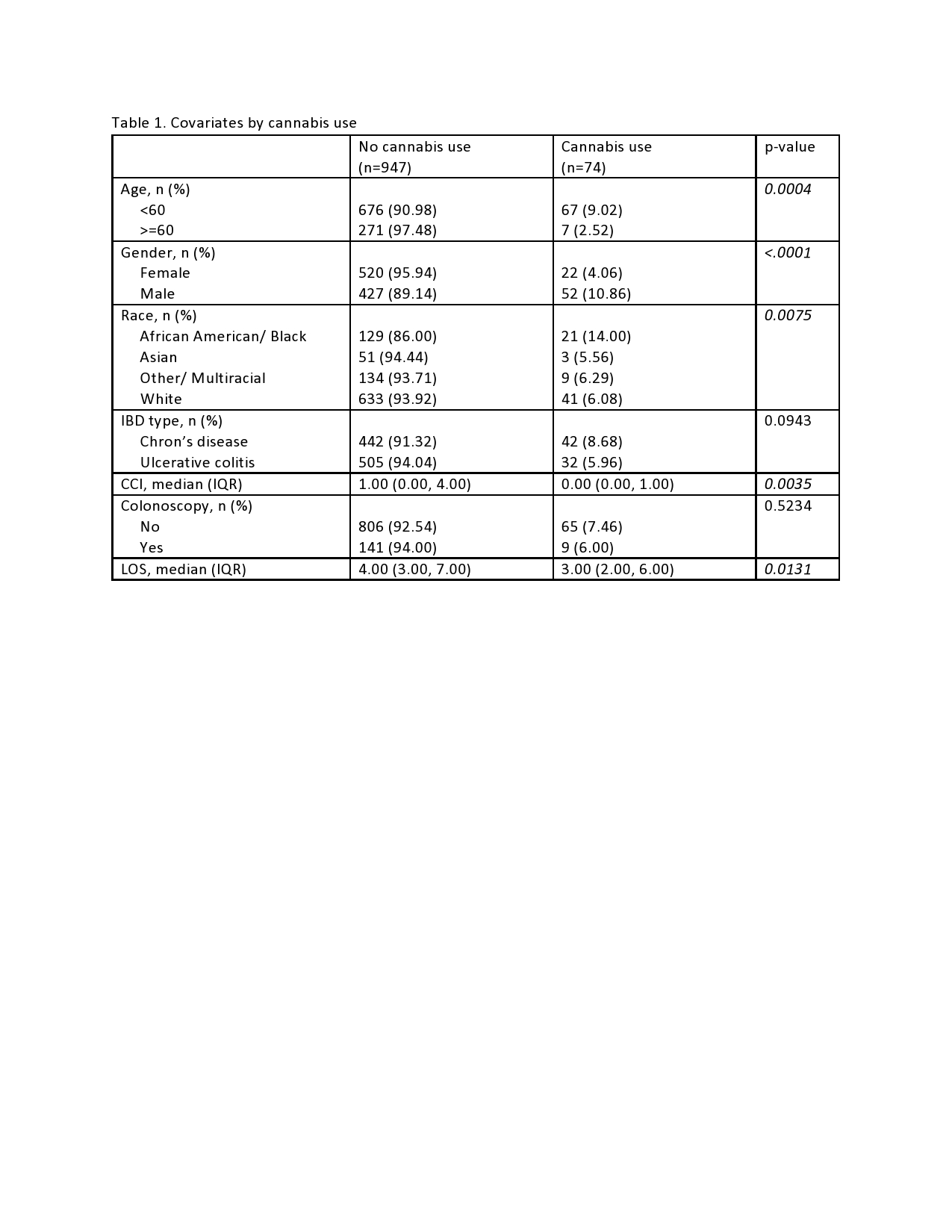
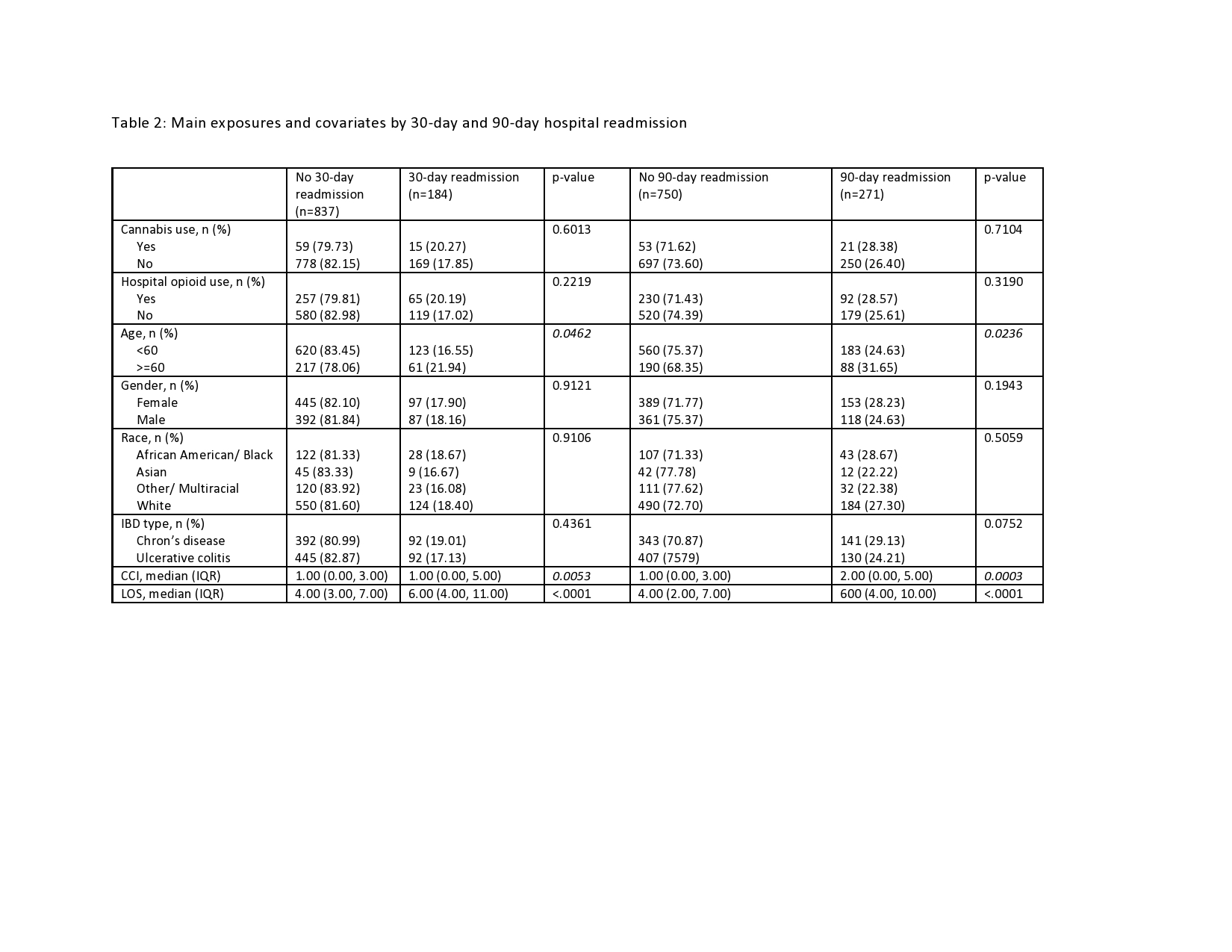
Results: A total of 1021 patient admissions met inclusion criteria; 484 (47.40%) with Crohn’s disease and 542 (53.09%) female. Pre-admission cannabis use was reported by 74 (7.25%) patients, who were younger and more likely to be male and African American than non-users, Table 1. 184 (18%) patients were readmitted by 30 days and 271 patients (26.5%) by 90 days, Table 2. Those older than 60 years, with increased LOS on index hospitalization and higher CCI, but not cannabis use were more likely to be readmitted within 30 and 90 days. Cannabis use was not found to be associated with 30-day (OR: 1.17, 95% CI: 0.65, 2.11) or 90-day readmission (OR: 1.11, 95% CI: 0.65, 1.87) on univariable analysis, nor on the multivariable model adjusted for age, CCI, and LOS: 30-day (OR: 1.36, 95% CI: 0.74, 2.52) and 90 day readmission (OR: 1.31, 95% CI: 0.76, 2.26). Hospital opioid use was not associated with increased 30-day or 90-day readmission on either univariable or multivariable analysis.
Conclusions: Preadmission cannabis use was not associated with more frequent 30 or 90-day readmissions following an IBD exacerbation. It is suspected, but not proven, that this cannabis use continued post hospitalization, and did not impact risk of readmission. Future studies will need to track these patients following discharge to see if this is correct, and also to assess for other potential adverse effects of cannabis use.