Background: Somatic Symptom and Related Disorders (SSRD) is an umbrella term for a wide variety of disorders commonly encountered in the inpatient pediatric setting, including conversion disorder, amplified pain syndrome, and psychogenic non-epileptiform seizures. These patients can be high utilizers of medical resources. The hospitalist is often charged with ruling out a medical diagnosis and then disclosing the possibility of a psychological basis for the physical symptoms. We have found this traditional approach often leads to the family’s response of “You think this is all in her HEAD?” followed by loss of the therapeutic alliance. We observed a variable approach both within our division, and by our subspecialist colleagues. The literature has no clear guidelines for the hospitalist to tackle these complex clinical scenarios.
Purpose: We created a Clinical Pathway (CP) to standardize a novel, multi-disciplinary approach to patients with suspected SSRDs. Key features of the CP include appropriate patient selection, standardized communication, early introduction of psychiatry, subspecialty buy-in, and a scripted “informing meeting” involving the patient, family and multidisciplinary team.
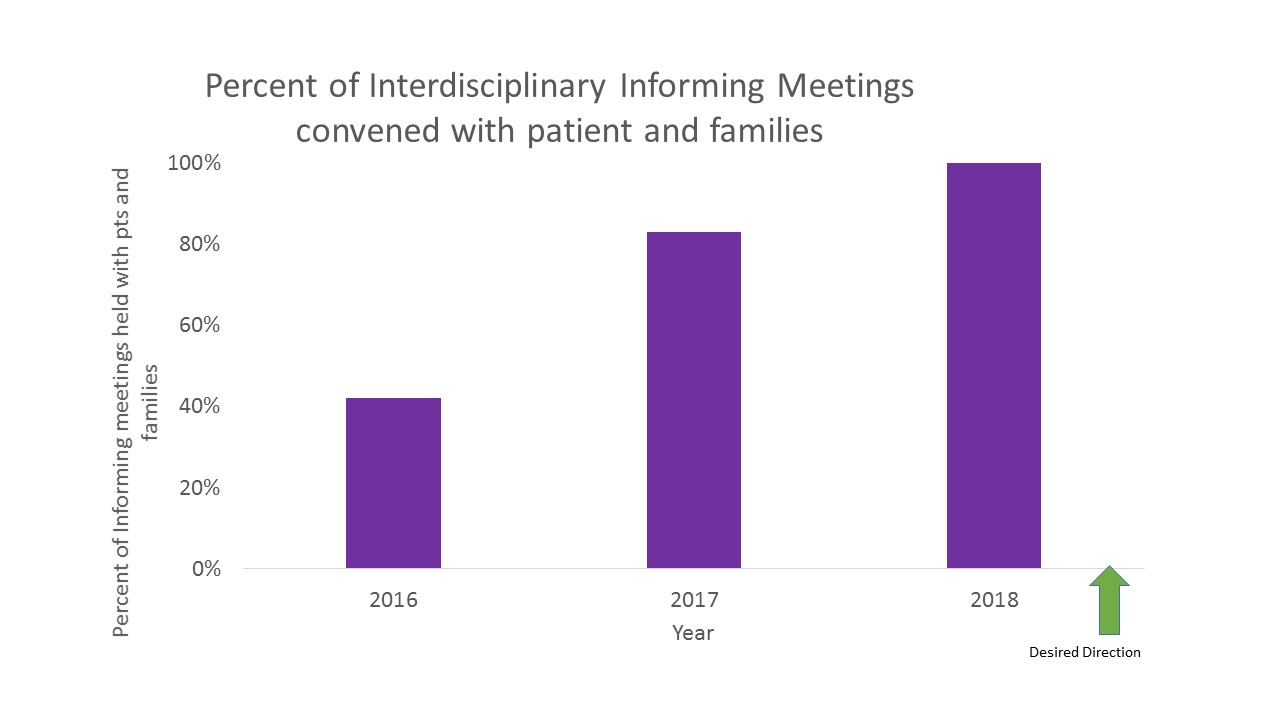
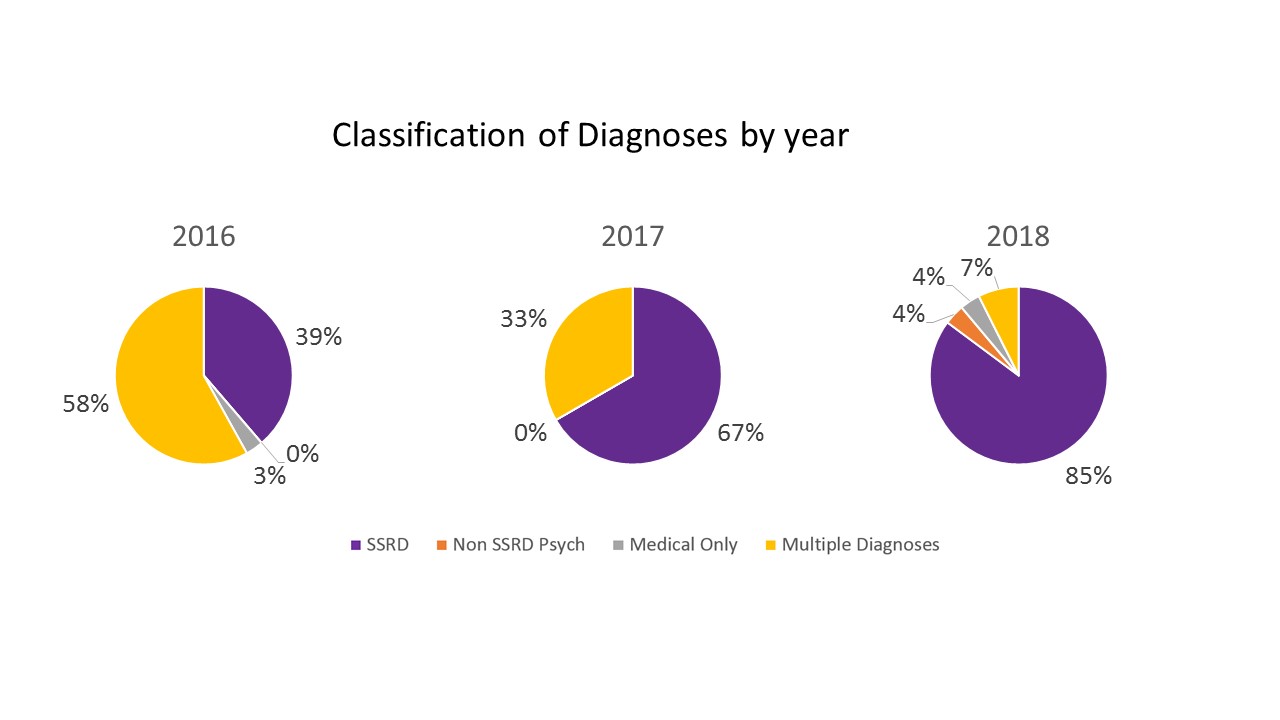
Description: A retrospective review of our electronic medical record was performed to identify patients who presented with SSRDs from 2016-2018. The CP was implemented in March 2017. An EPIC SmartPhrase capturing the content of the informing meeting was added in January 2018. Process measures included recording of diagnoses involved, whether the informing meeting took place, and percent of patients who exited the pathway with a medical diagnosis. The most frequent diagnoses were conversion disorder, pain amplification syndrome, and anxiety disorder. Over time, we increased the use of an informing meeting to 100% of all SSRD admissions. These informing meetings led to fewer medical diagnoses, and increased SSRD diagnoses. Only one patient exited the pathway, suggesting pediatric hospitalists are well equipped to identify patients likely to have an SSRD on admission.
Conclusions: The inpatient setting is a challenging arena to care for patients with SSRDs. Historically, providers have exhaustively ruled out medical causes in order to allow for an SSRD to be a diagnosis of exclusion. We challenged this model by creating a CP that acknowledges SSRD on the differential diagnosis at the time of admission. This innovative approach destigmatizes the behavioral health aspects, and works to minimize unnecessary or invasive testing by revealing mental health vulnerabilities earlier in the hospitalization. Our CP shows promising impact in identifying the population, and improving care through enhanced communication. This CP has standardized our approach to a challenging diagnosis, provided uniform language to avoid miscommunication, clarifies a psychiatric diagnosis as the primary cause of the presenting symptoms, and has unified the multidisciplinary team around optimal care for children with SSRDs.