Background: Individuals with autoantibodies against melanoma differentiation-associated protein 5 (MDA-5) are reported to have a significant risk of developing rapidly progressive and fatal interstitial lung disease (ILD) in clinically amyopathic dermatomyositis patients (CADM). Previous cohort studies of dermatomyositis patients who have been systematically evaluated for the presence of anti-MDA5 antibodies and associated clinical features and outcomes have been performed largely in the Asian, generally Japanese population, or Caucasian patients in North American studies. Available reports suggest rates of CADM and ILD may be lower in Caucasian predominant MDA-5 cohorts compared to Japanese groups. Additionally, association between rapidly progressive interstitial lung disease (RP-ILD) and MDA5 was variable in these North American studies. The goal of this study is to describe the clinical findings and outcomes of a pre-dominantly black cohort in anti-MDA5 associated ILD and the rapidly progressive variant.
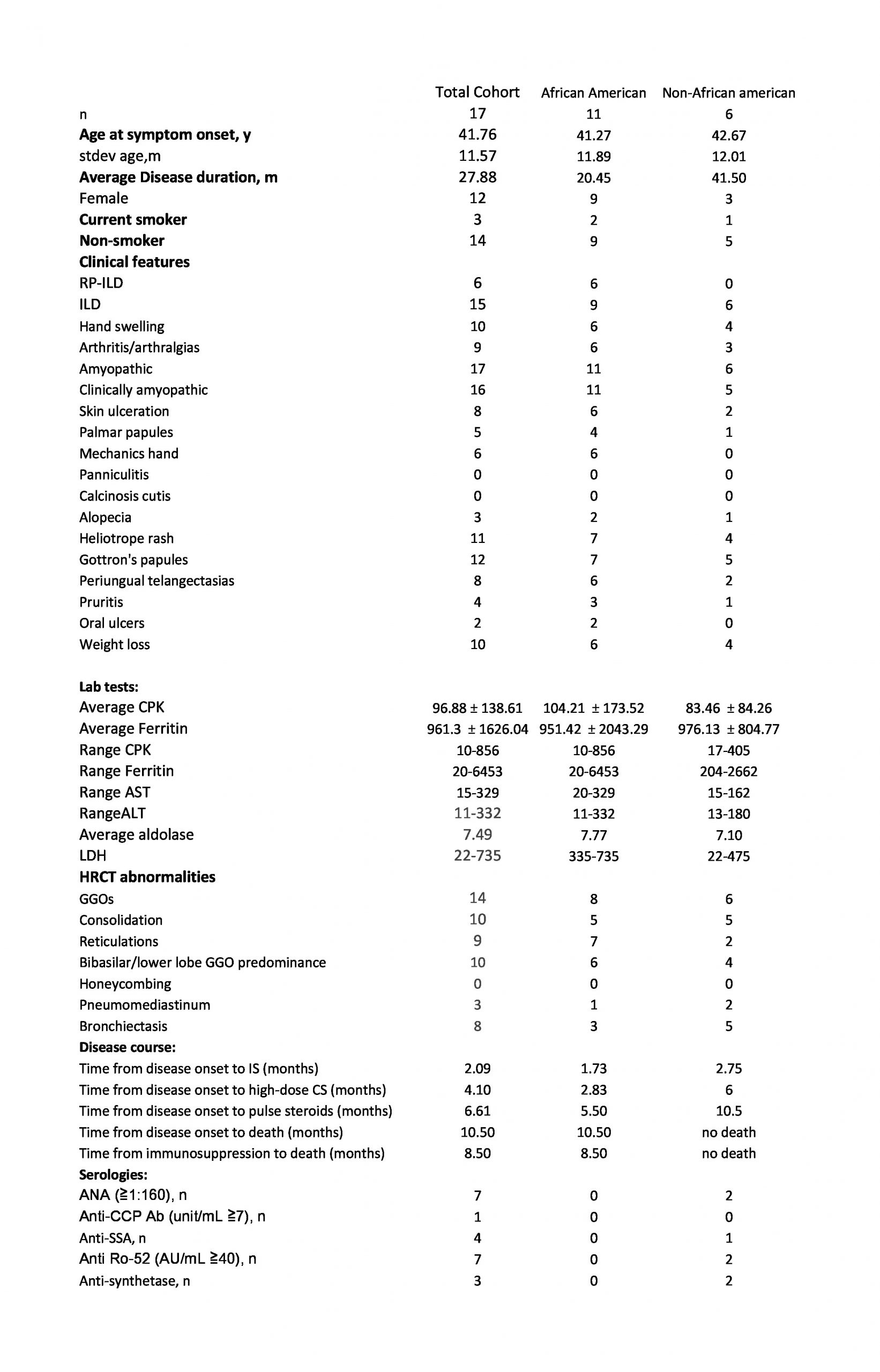
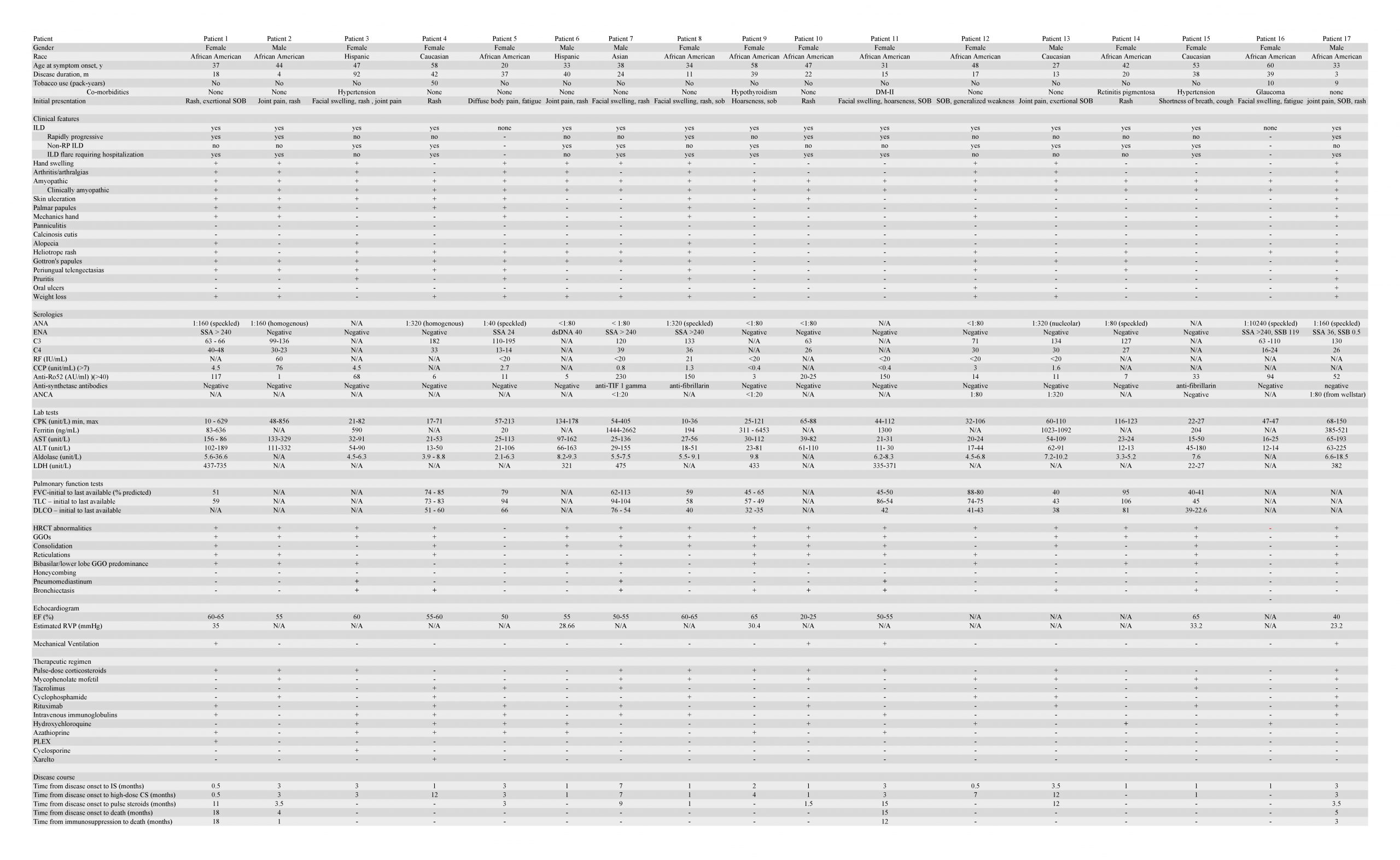
Methods: This retrospective cohort study identified 17 patients with CADM who had anti-MDA5 autoantibodies. Clinical characteristics, high-resolution computed tomography data, lab test results, presence of additional myositis autoantibodies (MAAs), and response to therapy and treatment outcomes were compared between 2 subgroups: black and non-black patients. MDA5 autoantibodies were measured by qualitative immunoprecipitation, Quantitative Bead Assay, and Line Blot Immunoassay.
Results: Among 17 patients with CADM and anti-MDA 5 autoantibodies identified between 2013 and 2020, 15 (88%) developed ILD with 6 patients (40%) having the rapidly progressive variant. Out of the pre-dominantly black cohort (11 of 17 patients), 6 (55%) patients had at least one additional MAA. Within the black cohort, 5 patients were positive for ANA, 1 for anti-CCP, 3 for anti-SSA, 5 for anti-Ro52, and 1 for anti-synthetase antibodies. Black patients exhibited a higher prevalence of MAAs when compared to the non-black cohort. All 6 patients with RP-ILD presented in the black sub-group. Average ferritin levels in black (951±2043) and non-black (976±805) patients were both elevated. Average values of CPK, aldolase, ferritin, FVC, and TLC did not differ significantly between black and non-black patients, but the majority of patients with anti-MDA5 antibody alone (4 of 5) developed ILD but not RP-ILD. Three out of four patients who died developed RP-ILD and all four had additional MAAs; time from initial symptoms to death ranged from 4 to 18 months. All survivors except one received hydroxychloroquine and/or mycophenolate mofetil as part of induction and/or maintenance therapy.
Conclusions: Black patients with anti-MDA5 positive DM exhibited many of the key phenotypic findings in other MDA5 positive DM populations. However, in our cohort, there was a notably increased incidence of RP-ILD and mortality among Black patients compared to non-Black patients. These potential phenotypic variations should be explored further as they can have implications for appropriate evaluation and treatment. Anti-MDA5 positive patients with CADM who are black have a higher prevalence of co-existent MAAs portending a poorer prognosis and a potentially greater predilection of developing RP-ILD than their non-black counterparts. Patients with anti-MDA5 antibodies alone generally have milder forms of ILD whereas coexistent MAAs serve as a possible marker for less favorable prognoses in anti-MDA5 positive patients with CADM.