Background: In medical care for older patients, the presence of potentially inappropriate medications (PIMs) is associated with increased adverse outcomes [1, 2]. A wide range of medications with anticholinergic properties affects cognitive states of older patients have been regarded as PIMs [1, 3]. We purposed to assess clinical impact of anticholinergic cognitive burden on clinical outcomes of older patients admitted via emergency department in a single, hospitalist-operated medical unit of a tertiary hospital in Korea.
Methods: By retrospective review of medical records, we enrolled patients 65 years of age or older who were admitted to hospitalist-operated medical unit via emergency department between February 2018 and October 2019. We assessed the anticholinergic cognitive burden (ACB) score of each patient by investigating the patients’ medications during hospitalization, and classified patient into those with an ACB score of 3 or higher and those with lower than 3. Length of stay, unplanned intensive care unit (ICU) admission, in-hospital mortality and unexpected readmission within 30 days were analyzed as clinical outcomes.
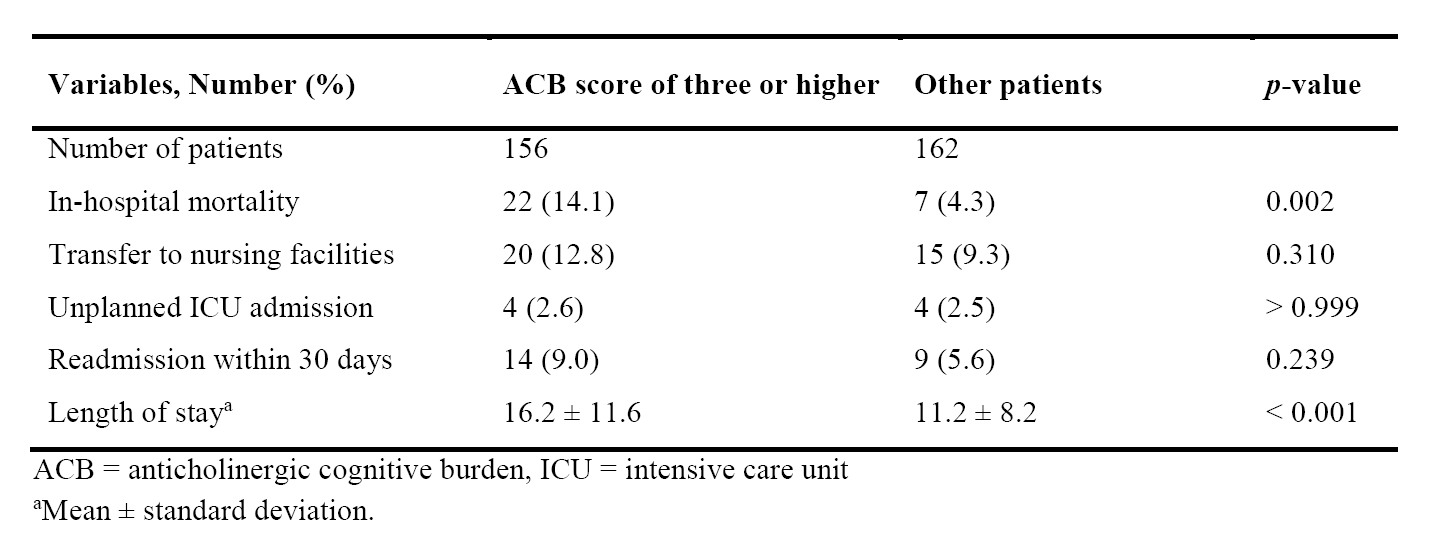
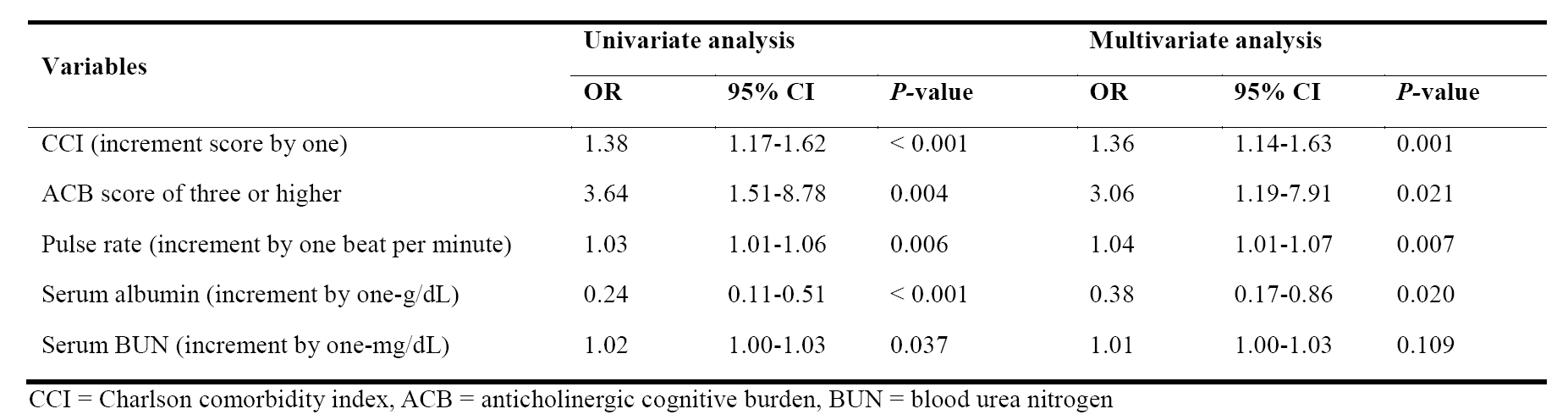
Results: Among 318 patients, patients taking five or more drugs were 240 (75.5%), and mean ACB scores was 3.1 points. There were 156 patients (49.1%) with an ACB score of 3 or higher, who considered to have a high anticholinergic burden. Patients who had high anticholinergic burden were taking more medications than patients who did not (mean, 9.0 VS. 7.8). Compared to patients who did not, patients who had an ACB scores of 3 or higher showed higher in-hospital mortality rate (14.1% VS. 4.3%; P = 0.002) and longer hospital stays (mean length of stay, 16.2 ± 11.6 days VS. 11.2 ± 8.2 days; P < 0.001). (Table 1) In regression analysis, Age, men, or number of medications were not associated with in-hospital mortality. In univariate model, five variables including CCI score, ACB score of 3 or higher, admission pulse rate, initial serum albumin or BUN level on admission were predictors of in-hospital mortality. After adjusting for confounding factors, ACB score of 3 or higher was an independent predictive factor for in-hospital mortality (Odds ratio [OR], 3.06, 95% confidence interval [CI], 1.19-7.91; P = 0.021). In addition, a higher CCI score, higher pulse rate, and a lower serum albumin level were also predictive factors of in-hospital mortality (Table 2).
Conclusions: In this study, we found that older patients admitted via emergency department had high prevalence of polypharmacy and also are exposed heavily to medications with anticholinergic properties. Analysis showed that anticholinergic burden, not polypharmacy per se, was associated with in-hospital mortality.