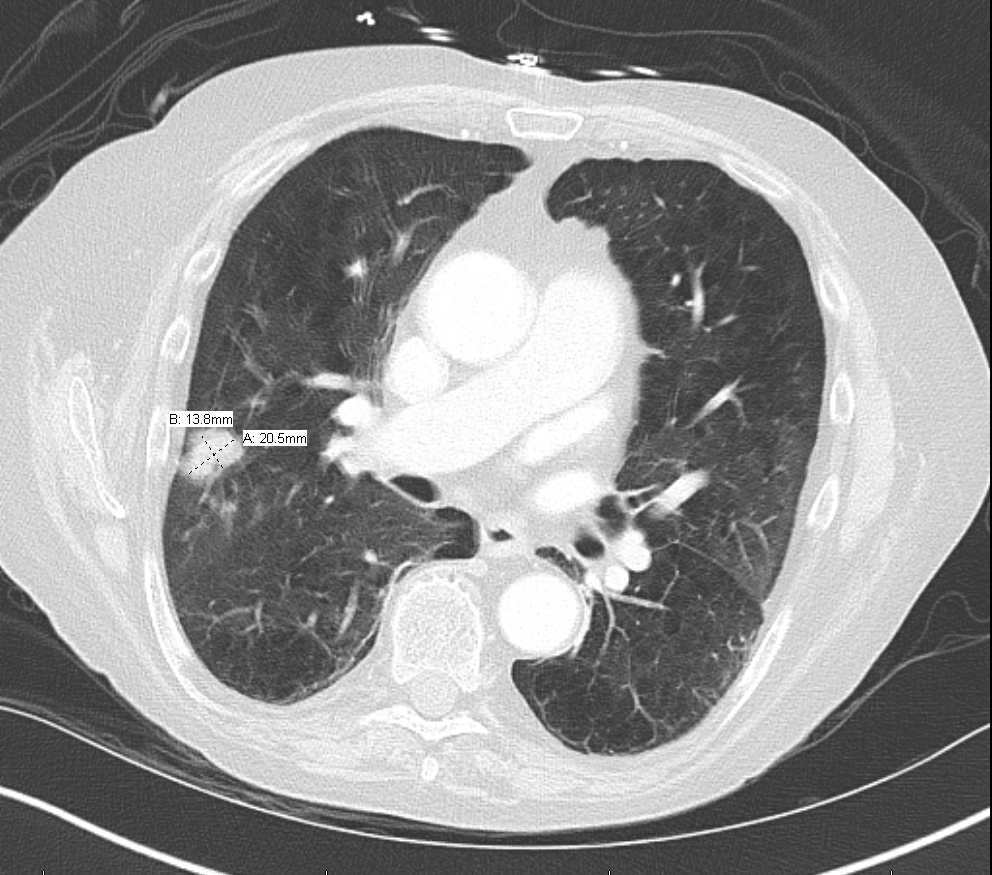
Case Presentation: 71 year old man with known medical history of atrial fibrillation (on Rivaroxaban), severe chronic obstructive pulmonary disease, diabetes mellitus, history of perforated diverticulitis with surgery and colostomy one year ago complicated with recurrent methicillin-resistant Staphylococcus aureus (MRSA) infections and prolonged hospitalizations, including MRSA pneumonia and respiratory failure one month ago, presented to the emergency department due to one week history of decreased vision in left eye and now near total loss of vision with ophthalmodynia. Of note, he recently was diagnosed with a COPD exacerbation and started on prednisone taper. On admission, the patient was febrile, 38.9C. Physical examination showed an ill appearing man with functioning colostomy. Eye exam revealed injected conjunctiva with significantly decreased visual acuity. Laboratory studies were remarkable for lactate of 1.9. Chest radiograph (CXR) showed 15 mm mass in right lung and computerized tomography (CT) chest showed three right lung nodules, largest measuring 14x 21 mm. Patient was started on broad spectrum antibiotics; vancomycin and piperacillin and tazobactam. Ophthalmology was consulted and he underwent a vitrectomy, vitreous biopsy, anterior chamber wash out and intravitreal vancomycin and ceftazidime. A large pre retinal abscess was also found. Blood cultures were obtained and found to be negative. Vitreous humor culture grew one colony of aspergillus fumigatus. Transthoracic echocardiogram (TTE) was negative for vegetations. CT of the chest, abdomen, and pelvis was ordered to determine the source of infection and showed a pelvic abscess near the stoma. Cultures of this were positive for Escherichia coli and Bacteroides. Further laboratory studies were positive for serum Beta-D-glucan >500. Serum galactomannan assay was negative. CT scan brain was negative. Patient was switched to cefepime and metronidazole and started on voriconazole. He also received intravitreal voriconazole. Patient was discharged on oral voriconazole, cephalexin and metronidazole for six weeks. On subsequent outpatient follow up, his vision was significantly improved.
Discussion: Disseminated aspergillosis occurs almost exclusively in immunosuppressed patients, most commonly in those with acute leukemia and in recipients of organ transplants. Neutropenia, prolonged antibiotic therapy, and the use of cytotoxic and/or corticosteroid drugs are factors that appear to predispose patients to this infection (1).Fungal endophthalmitis is infrequent and results in poor visual outcomes. Broad-spectrum systemic antifungal therapy with or without intravitreal antifungal drugs is recommended. The prognosis depends upon the virulence of the organism, extent of intraocular involvement and the timing of interventions. Prompt therapy following early diagnosis helps to reduce significant visual loss.
Conclusions: Aspergillus endophthalmitis is a rare inflammatory disorder that can result in irreversible destruction of the eye and loss of vision. Acute endophthalmitis is a medical emergency that is often due to the introduction of organism via surgery or trauma but it can also occur hematogenously in immunosuppressed patients . Prompt recognition and treatment of this condition with antifungal medications can be potentially vision saving, as in our case.