Background: Falls are associated with significant morbidity and increased healthcare expenses for hospitalized patients. There are hundreds of thousands of inpatient falls every year. There are multiple validated scores to guide the need of imaging for patients presenting to ED after, but no such score exists for hospitalized patients who suffer a fall event. This study was done to analyze different predictors of falls, evaluate different factors associated with post-fall imaging, and also to determine their correlation to positive versus negative imaging findings.
Methods: Single Center Retrospective Cohort analysis of inpatient falls from July 2018 to June 2020 done as the pilot study of a quality improvement project. Data was collected from the hospital inpatient adverse event reporting system and analyzed for age, gender, fall risk score at baseline, time and mechanism of fall, administered medications, and fall related imaging.
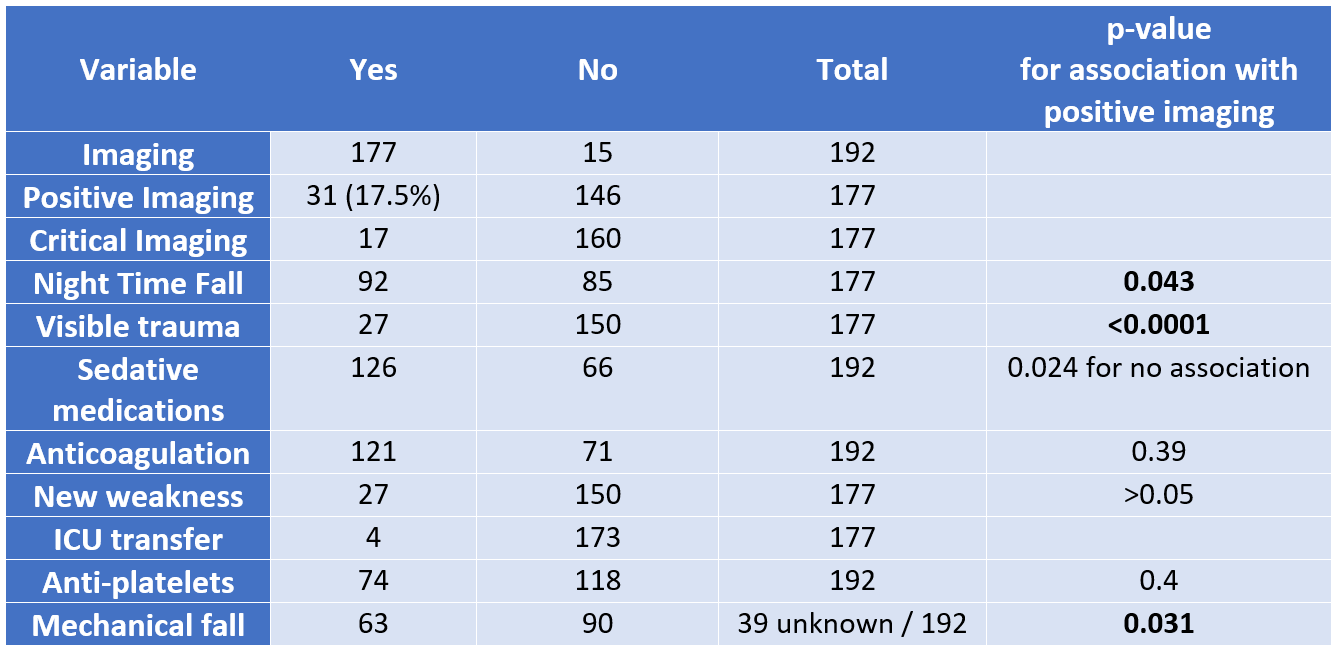
Results: Of 192 falls over 24 months, there were 83 females and 109 males with mean age of 68.4 year (SD 17.3, range 20-96 years). 94 (49%) falls occurred during day and 98 (51%) during night. Patients with night-time falls were more likely to get CT head (92 (94%) vs 80 (85%) in day, p-value 0.047). CT Head was more likely to be ordered for males (OR- 3.9), at night (OR 6.7), and less likely for witnessed falls (OR 0.19). Positive findings in neuro-imaging were more likely to be associated with night falls (OR 2.3, p=0.043), visible trauma (OR 5.5, p<0.0001), mechanical fall (OR 5, p=0.031), while less likely to be associated with sedatives (OR=0.4, p =0.024). There was no statistically significant difference between likelihood of falls during day-time vs night-time, but night falls were more likely to get imaging, and have positive results (p=0.002). 94% of the patients with high fall risk assessment score got post-fall CT head, 16% were positive, as compared to 21% positive scans in patients with low fall risk scores (p>0.1). 14 out of 31 patients with positive CT imaging were on anti-platelet therapy, but association was statistically not significant (possibly due to small sample size) (p=0.4). Therapeutic anticoagulation was not associated with positive imaging (p=0.39). Visible trauma was associated with higher chance of positive imaging (p<0.0001), while there was no statistically significant association of new weakness with positive imaging. Of our cohort of patients, more than 50% did not meet criteria for imaging as per Canadian Head Trauma CT scoring.
Conclusions: Our findings show that although multiple clinical scores exist to guide imaging in outpatient or emergency settings, no such scores are followed closely in hospitalized patients since they are not validated in this setting. We suggest a larger QI study to implement new guidelines for CT Head after inpatient falls, with factors such as time of fall, visible trauma, mechanism of fall, and coagulopathy included as predictors of positive imaging. Other factors like age, gender, use of sedative medications, and baseline fall score should be given lower points in scoring system.