Background: Most cases of pneumonia in older people are aspiration pneumonia,[1] and the prognosis among patients hospitalized for aspiration pneumonia is very poor.[2] After being hospitalized for aspiration pneumonia, a certain number of patients become unable to take orally, and some chronic conditions are reported to be negatively associated with the retrievement of oral intake.[3] Multimorbidity is defined as the co-occurrence of two or more chronic conditions within a person and is quite common among older people in developed countries.[4] Degenerative/mental health, malignant/digestive/urological/hematological, and cardiovascular/metabolic patterns are known as multimorbidity patterns in the older general population.[5] However, multimorbidity patterns in patients with aspiration pneumonia are unknown. Therefore, this study aimed to investigate multimorbidity patterns in patients hospitalized for aspiration pneumonia and their association with survival discharge with oral intake.
Methods: We retrospectively identified 269 patients aged ≥ 65 years hospitalized for aspiration pneumonia at a tertiary care hospital from April 2009 to September 2014. Data were extracted from the medical record including patient age, sex, body mass index (BMI), Eastern Cooperative Oncology Group Performance Status (PS) before admission, chronic conditions, laboratory data, imaging, nutritional pathway at discharge, discharge place, and mortality. Chronic conditions with a prevalence among the patients of > 3% were included in assessing multimorbidity. Multimorbidity patterns were identified by hierarchical cluster analysis. Multivariable modified Poisson regression analyses with age and sex as covariates were performed to investigate the association between the presence or absence of each multimorbidity pattern and survival discharge with oral intake. The association between each multimorbidity pattern and mortality was also analyzed. The institution’s ethics committee approved the study protocol and they waived the informed consent, as the nature of the retrospective design.
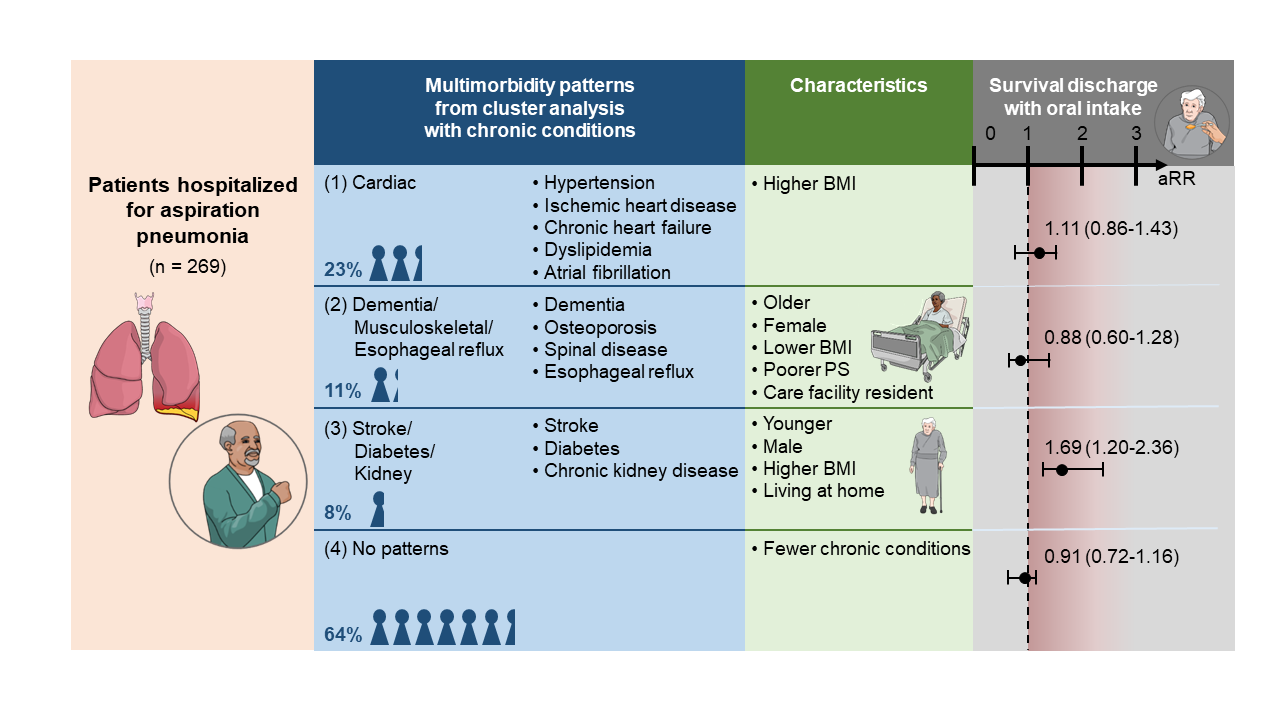
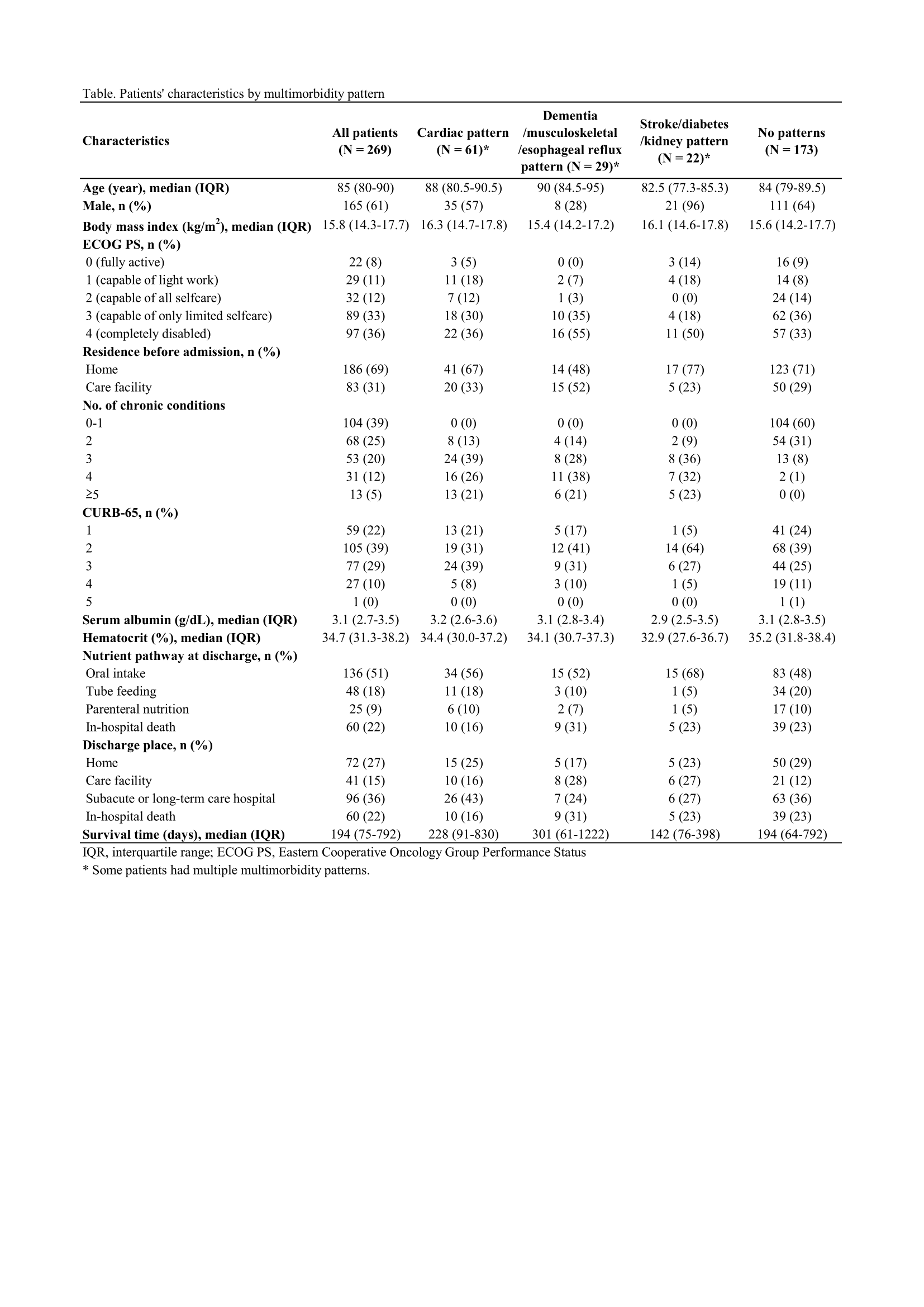
Results: The median age of the patients was 85 years, the median BMI was 15.8 kg/m2, 61% were male, 36% had PS of 4, in-hospital mortality was 22%, and 51% were taking orally at survival discharge. During the follow-up period, 81.8% of all patients died, and the median survival time was 194 days. There were 15 chronic conditions with a prevalence of > 3%. The prevalence of multimorbidity was 77%. Three multimorbidity patterns were identified: (1) cardiac, (2) dementia/musculoskeletal/esophageal reflux, and (3) stroke/diabetes/kidney. Patients with dementia/musculoskeletal/esophageal reflux pattern tended to be older females with poorer PS and lower BMI in care facilities. In contrast, there was a trend for patients with stroke/diabetes/kidney pattern to be younger males with higher BMI living at home (Table). Stroke/diabetes/kidney pattern was associated with survival discharge with oral intake (adjusted risk ratio = 1.69, 95% confidence interval: 1.20-2.36) (Figure). There were no patterns significantly associated with mortality.
Conclusions: Three multimorbidity patterns were identified in older patients hospitalized for aspiration pneumonia. Stroke/diabetes/kidney pattern was associated with survival discharge with oral intake. Patients with the pattern may be good candidates for aggressive nutrition and rehabilitation therapy to retrieve oral intake.