Background: Paracentesis is a common procedure for patients with decompensated cirrhosis. In patients with cirrhosis and superimposed renal impairment, clinicians may hesitate to perform a large volume paracentesis, given concerns of intraabdominal fluid shifts resulting in further renal dysfunction. In this study, we aimed to answer whether greater ascites fluid removal was associated with 48-hour creatinine change in a cohort with concomitant decompensated cirrhosis and renal impairment.
Methods: We conducted a retrospective, single-center cohort study at Parkland Health of patients admitted with concomitant cirrhosis and elevated creatinine (>1.20mg/dL) who underwent paracentesis between 2021-2022. Patients were excluded if they had end-stage renal disease, suspicion for hepatorenal syndrome (defined by albumin administration prior to paracentesis), had multiple paracentesis during admission, or did not have a 48-hour post-procedure creatinine level. Data were extracted by chart review and verified by two study personnel. The primary exposure was paracentesis volume, and the primary outcome was a change in creatinine from admission to 48 hours. Relevant covariates were determined a priori based on a conceptual model of factors affecting paracentesis volume and creatinine change. Because some patients were hospitalized multiple times during the study period, a fully adjusted mixed effects linear regression model accounting for repeated measures was utilized to assess the association between paracentesis volume and change in creatinine. An exploratory analysis was conducted to evaluate whether adding post-procedural albumin administration into the primary model would attenuate the association between volume removal and creatinine change.
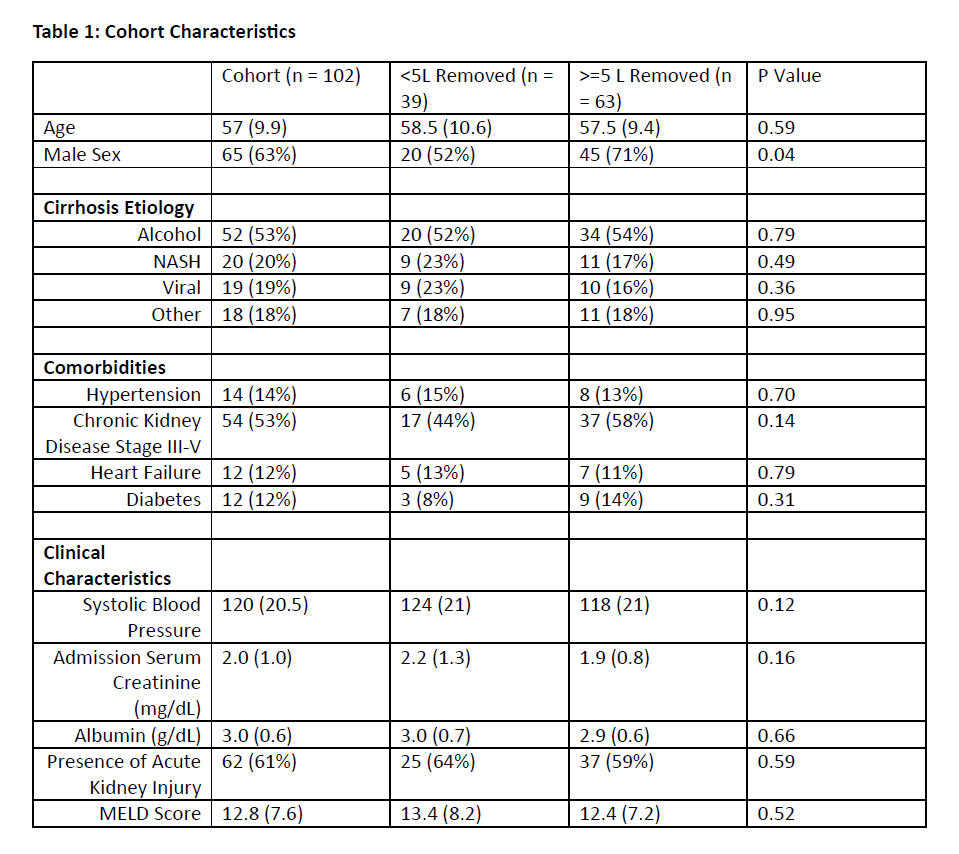
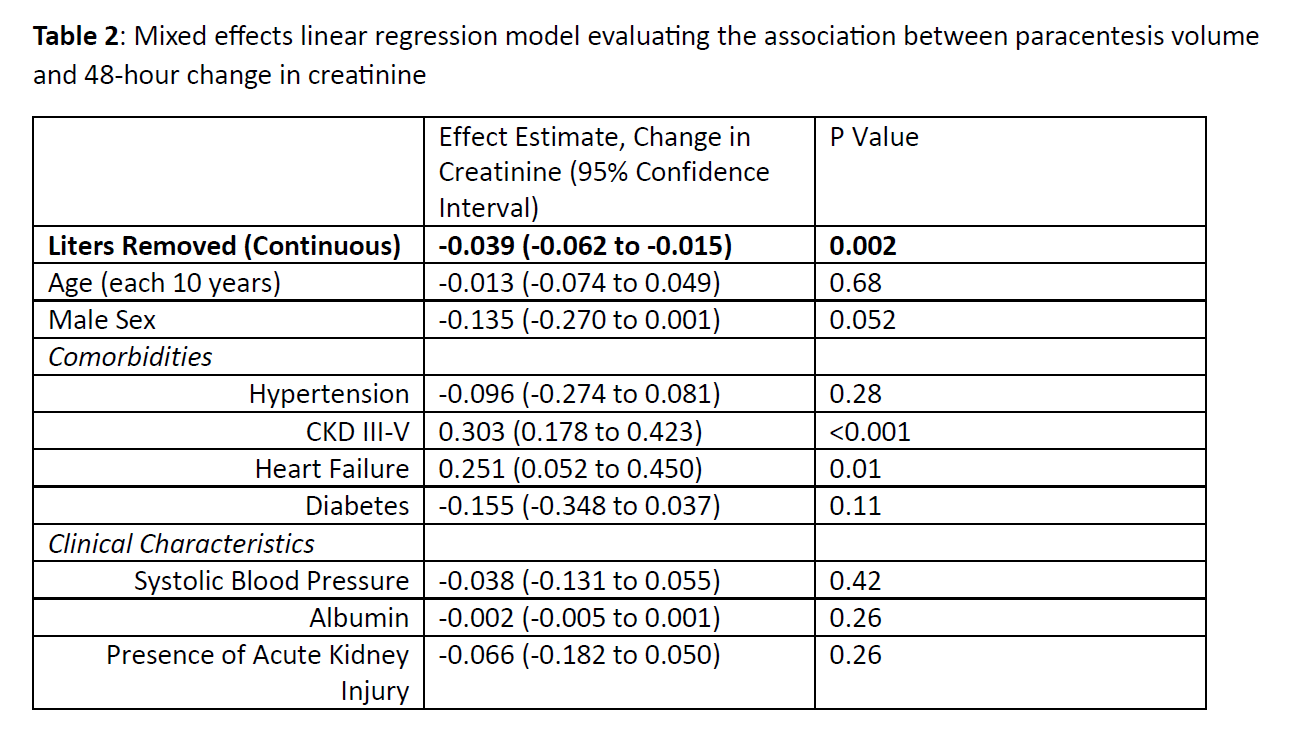
Results: 102 patients were included in this study (mean age 57 years, 63% men) (Table 1). The mean pre-procedure creatinine was 2.0 mg/dl, and the mean MELD score was 12.8 (SD 7.6). Over half of patients (53%) had chronic kidney disease stages III-V and 61% presented with acute kidney injury. The mean and median paracentesis volumes were 5.4L (SD 2.5) and 5L (IQR 4 to 7L), respectively. Sixty-three patients had over 5L removed, compared with 39 patients with less than 5L removed. Men were more likely to have 5L removed than women (P = 0.04). In a fully adjusted mixed linear regression model, each liter removed was associated with a reduction in 48-hour serum creatinine (-0.04 mg/dL per liter removed [95% CI: -0.06 to -0.02, P=0.002] (Table 2). When post-procedural albumin administration was added to the fully adjusted model, albumin administration was not associated with a reduction in 48-hour creatinine (estimate 0.01 mg/dL (95% CI: -0.14 to 0.16, P=0.89) and the association of paracentesis volume remained relatively unchanged (-0.03 mg/dL 95% CI: -0.06 to -0.01, P=0.02).
Conclusions: We find that larger volume ascitic fluid removal is associated with greater reductions in 48-hour serum creatinine. This finding remained consistent after accounting for post-procedural albumin administration. Given the retrospective, single-center nature of this study, we could not account for confounding by indication or address limitations in generalizability. This study provides early evidence to suggest that conservative paracentesis fluid removal in patients with cirrhosis and renal impairment may be unnecessary. Randomized studies assessing ascites volume removal and subsequent renal function should be pursued.