Background: Efforts to advance health equity in the outpatient setting include routine screening for social determinants of health, expanded access to addiction treatment, and addressing pharmaco-equity. However, the question of how to advance health equity for patients who are hospitalized has been underexplored. We sought to understand hospitalists’ perspectives on health equity needs and innovations.
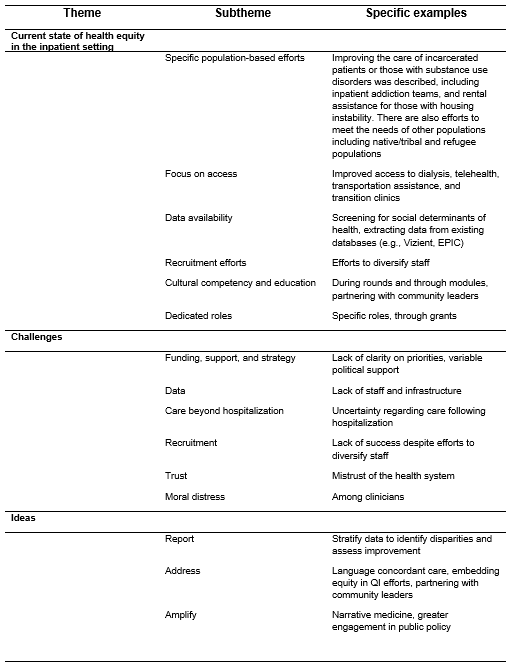
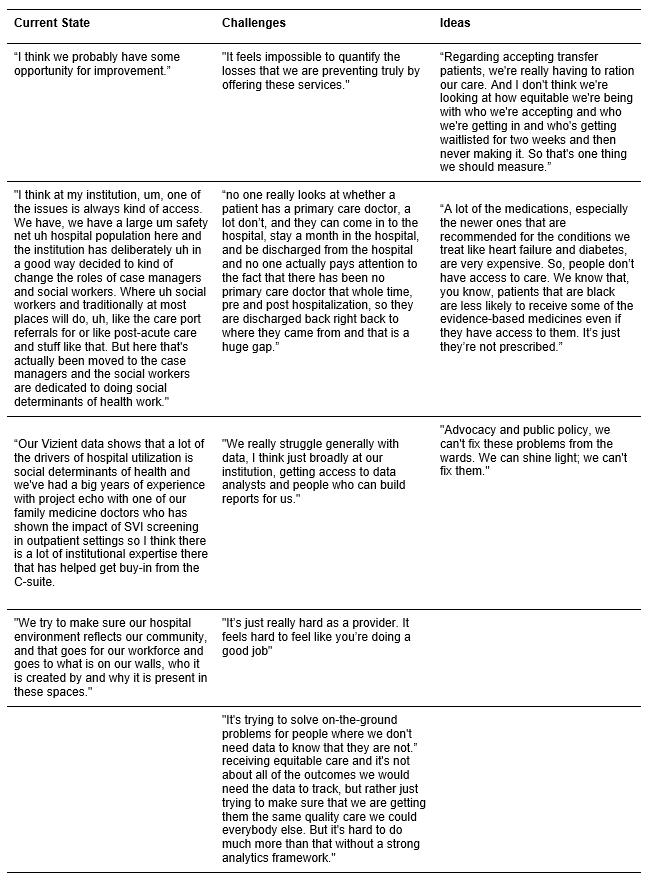
Methods: We conducted semi-structured focus groups with members of HOMERuN – a U.S. collaborative of hospital medicine groups partnering to improve healthcare delivery. Focus groups focused on 1) the current state of health equity, 2) challenges to incorporating health equity, and 3) ideas to measure, report, and address health equity all in inpatient settings. Focus groups were recorded and transcribed. Rapid qualitative analysis methods were used to explore themes and subthemes. We report the preliminary findings here.
Results: Twenty-one hospitalist physicians and physician trainees participated in the focus groups. Key themes emerged across the three designated domains. (Tables 1 and 2)Many hospitals are investing in ways to improve access to equitable care, both within and outside the hospital. Initiatives range from recruitment and retention efforts to diversify staffing to clinical care models like inpatient addiction medicine consult services and post-acute care transitional clinics for uninsured patients. Many are focusing on historically marginalized populations, including patients experiencing incarceration, homelessness & housing instability, or those with substance use disorders. Participants shared increasing inpatient efforts to screen for social drivers of health as well as improving language access and support. There was a shared understanding that valid and reliable patient sociodemographic data was necessary for addressing improved health equity. Stratifying process and outcomes data by subpopulations was unanimously supported to proactively identify and address disparities in care. However, most participants also cited the variability of hospital-based infrastructures for data collection as a key barrier to measuring health equity-related outcomes. Similarly, a lack of funding and resources, including time for faculty and supporting staff (e.g., informaticists and data analysts), limited the scope and pace of equity work. Participants felt that in the current state, moving health equity work forward relies on passionate individuals volunteering. Potential consequences of these challenges for hospitalists were frustration and moral injury. Other challenges included recruiting and retaining a workforce that mirrored the local community and the dearth of resources to address the complexity of care following hospital discharge. Suggestions for future work included improved access to valid and reliable socio-demographic and social driver screen data, routine stratification by socio-demographics, and accessibility of these data (e.g., via electronic health record dashboards) to share and make actionable. Other ideas discussed included embedding equity into quality improvement, greater public policy engagement, focusing on patient education efforts, and utilizing narrative medicine to share the impact of these efforts.
Conclusions: Focus groups of hospitalists from across the country found that while progress is being made in addressing health equity in hospital medicine, the pace and scope are limited by funding and infrastructure barriers.