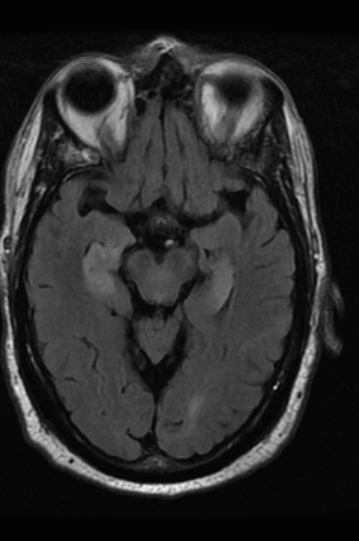
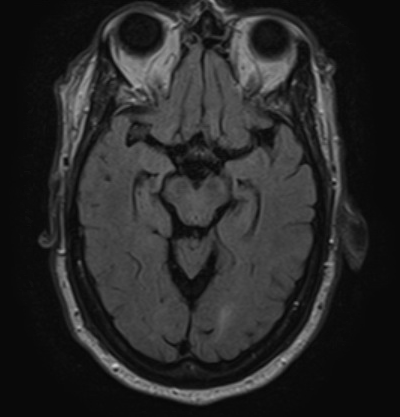
Case Presentation: A 74-year-old male with a past medical history of Stage III CKD and paroxysmal atrial fibrillation was initially taken to his PCP by his wife for changes in his mental status, trouble remembering things and following directions while driving. As his outpatient workup was ongoing, he also developed a fever with chills and was taken to the Emergency Department. In the ED, a complete blood count, the comprehensive metabolic panel were unremarkable. A lumbar puncture was performed, and empiric meningitis coverage was initiated. His cerebrospinal fluid (CSF) analysis revealed 4 nucleated cells, 0 RBCs, protein 44 mg/dl, and glucose 88 mg/dl. HSV 1/2 PCR came back negative and CSF cytology was negative for any malignant cells. An MRI showed bilateral hippocampal edema. A routine EEG revealed diffuse slow waves consistent with a mild encephalopathy and a 24-hour EEG did not reveal any subclinical seizures. A CT chest abdomen and pelvis was negative for any mass or lymph nodes concerning for malignancy. As an infectious workup was non-revealing and other causes were ruled out, with the concern for paraneoplastic or autoimmune encephalitis, the patient was started on high dose steroids and plasma exchange while results of antibodies for autoimmune and paraneoplastic encephalitis were awaited. After plasmapheresis and a course of steroids, the patient’s mental status began to slowly improve. He was discharged from the hospital and on a subsequent neurology office visit, his serum autoimmune encephalitis panel returned positive for anti-LGI 1 antibodies. Further management consisted of outpatient Rituximab infusion.
Discussion: Diagnosis of limbic encephalitis can be challenging and can present with symptoms of limbic dysfunction. In Anti-LGI1 LE, cerebrospinal fluid analysis is usually normal. In some cases, MRI may show signal changes in the medial temporal lobes and basal ganglia and PET scans may show a characteristic increase in the frontal-occipital gradient of cerebral glucose metabolism, which correlates with disease severity. However, a number of patients do not show abnormalities on MRI or PET.
Conclusions: A modest index of suspicion of limbic encephalitis should be kept in adults with altered mental changes. Early recognition and initiation of therapy can be crucial in the management of patients with autoimmune encephalitis and can prevent permanent cognitive impairment and damage. The therapeutic responsiveness of this condition reiterates the importance of diagnosing a reversible neurologic pathology. Treatment involves corticosteroids, intravenous immunoglobulin, and plasma exchange as well as immunomodulators like cyclophosphamide and rituximab with immunotherapy.