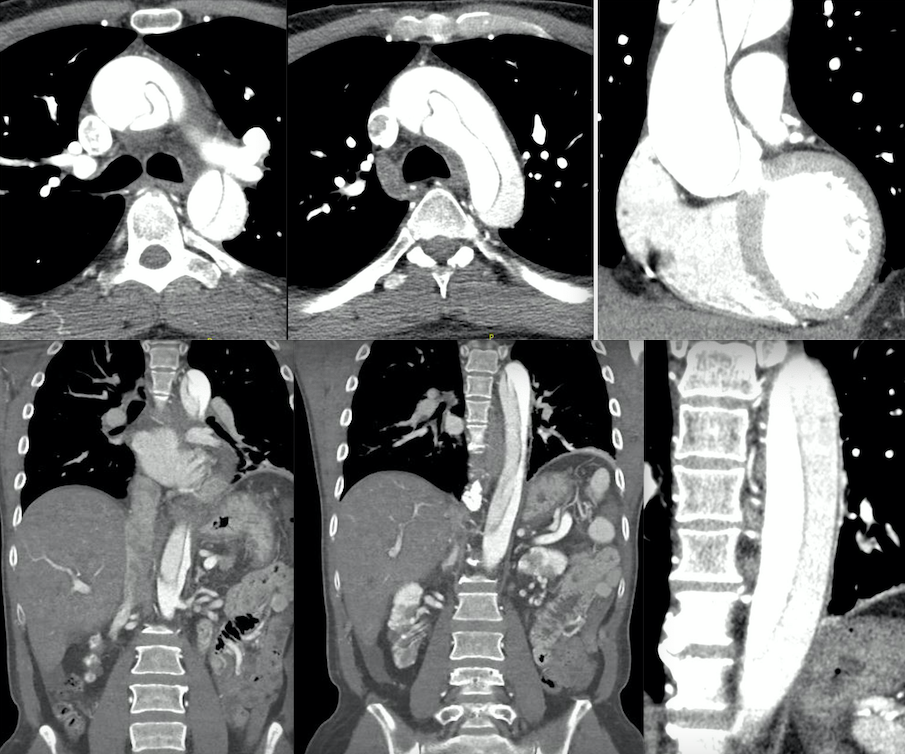
Case Presentation: A 59-year-old male with chronic renal insufficiency due to IgG4-related disease (on chronic steroid therapy) and autoimmune pancreatitis presented to the ER with lightheadedness and numbness of bilateral upper extremities after masturbation. He experienced urinary incontinence, but no loss of consciousness. EMS found him hypotensive and bradycardic (BP 84/50, HR 30s) and administered atropine and fluids. The patient was normotensive at outpatient visits and a never-smoker. He denied chest pain and the use of sildenafil or any other medications, drugs, or sexual enhancers.On exam, a loud systolic murmur was noted, which had never been documented on outpatient notes, along with thready symmetrical pulses and delayed capillary refill. Labs showed a lactate of 2.7 mmol/L, WBC count of 17.9 k/uL, and no change to chronically elevated BUN/Cr levels. A chest X-ray was unremarkable.The patient’s blood pressure was not responding to fluids. Given the unresponsive hypotension and leukocytosis in this immunocompromised patient, an infectious workup and empiric antibiotics were initiated. A transthoracic echocardiogram to assess the murmur and cardiac function was done the next day, revealing Type A aortic dissection, confirmed by CT angiogram showing extensive dissection from the aortic root, involving major arteries. The patient was transferred to the Coronary Care Unit, started on an esmolol drip, and underwent aortic repair with an uneventful postoperative course.
Discussion: Chronic corticosteroid use, which our patient was using for suppression of IgG4 disease, decreases collagen formation in vessel walls, increasing risk of aneurysm and dissection [1]. It also contributes to chronic arterial hypertension, stressing vascular structures and raising cardiovascular risk [2]. Increased capillary permeability may lead to fluid extravasation, impacting vascular function [3]. Careful monitoring is crucial for patients on corticosteroids.IgG4-related aortopathies caused by aortic inflammation due to elevated IgG4 levels often present with systemic symptoms like fever and malaise [4]. They can mimic infectious aortitis and other autoimmune diseases [5]. Corticosteroids are effective in reducing inflammation, but may not prevent severe complications like aortic dissection, especially if delayed [6], which complicates management even further given that the therapy for IgG4 disease can also directly contribute to aortopathy given its effects discussed earlier. Since patients with IgG4-related disease are at higher risk for aortopathies, there may be benefit in baseline and regular imaging surveillance [8] [9].
Conclusions: This patient lacked typical aortic dissection symptoms, such as chest pain which occurs in >90% of aortic dissection patients, initially obscuring diagnosis and delaying intervention. This underscores the importance of recognizing atypical presentations and the relation with corticosteroids and IgG4 disease. Despite being on corticosteroids for his IgG4-related renal disease, the patient developed aortopathy, emphasizing the limitations of steroid therapy in preventing such complications, even possibly contributing to them. This brings up the question of the need for routine screenings for complications, such as outpatient echocardiograms or CT angiograms. Recognizing unique risk factors and atypical manifestations associated with steroids and IgG4-related aortopathies is crucial for timely diagnosis and management to improve patient outcomes.