Case Presentation: A 91 year-old woman with congestive heart failure (CHF), chronic kidney disease, and morbid obesity was admitted with subacute shortness of breath. The patient’s CHF history was significant for no prior emergency department visits or hospitalizations attributed to CHF exacerbation. A recent transthoracic echocardiogram demonstrated moderate concentric left ventricular hypertrophy with a normal ejection fraction.
On examination, she had a respiratory rate of 18-22 with otherwise normal vital signs. She appeared comfortable, with mild tachypnea on exertion. She had normal cardiac and pulmonary auscultation and trace symmetric lower extremity edema; jugular venous pressure could not be assessed due to neck circumference. Labs showed creatinine 1.36 (baseline), negative troponin, and BNP 153 (ref. range <181). Chest x-ray demonstrated low lung volumes. A point-of-care ultrasound (POCUS) performed by an experienced hospitalist demonstrated an inferior vena cava of 1.3 cm and greater than 50% collapsible, difficult cardiac windows and bowel gas in the subcostal view but with grossly normal ejection fraction without pericardial effusion anteriorly, normal lung sliding, no pulmonary B-lines, and no pleural effusion.
Given the entirety of her POCUS examination, the patient was thought to be euvolemic. She was admitted in the evening and handed off to a new team the following day with the reported POCUS exam. However, based on symptoms and exam, she was given higher dose diuretics and subsequently developed acute rise in creatinine to 2.2. She was then treated with IV fluids and was ultimately discharged four days after admission after improvement in her renal function with diagnoses of deconditioning and acute kidney injury secondary to diuresis.
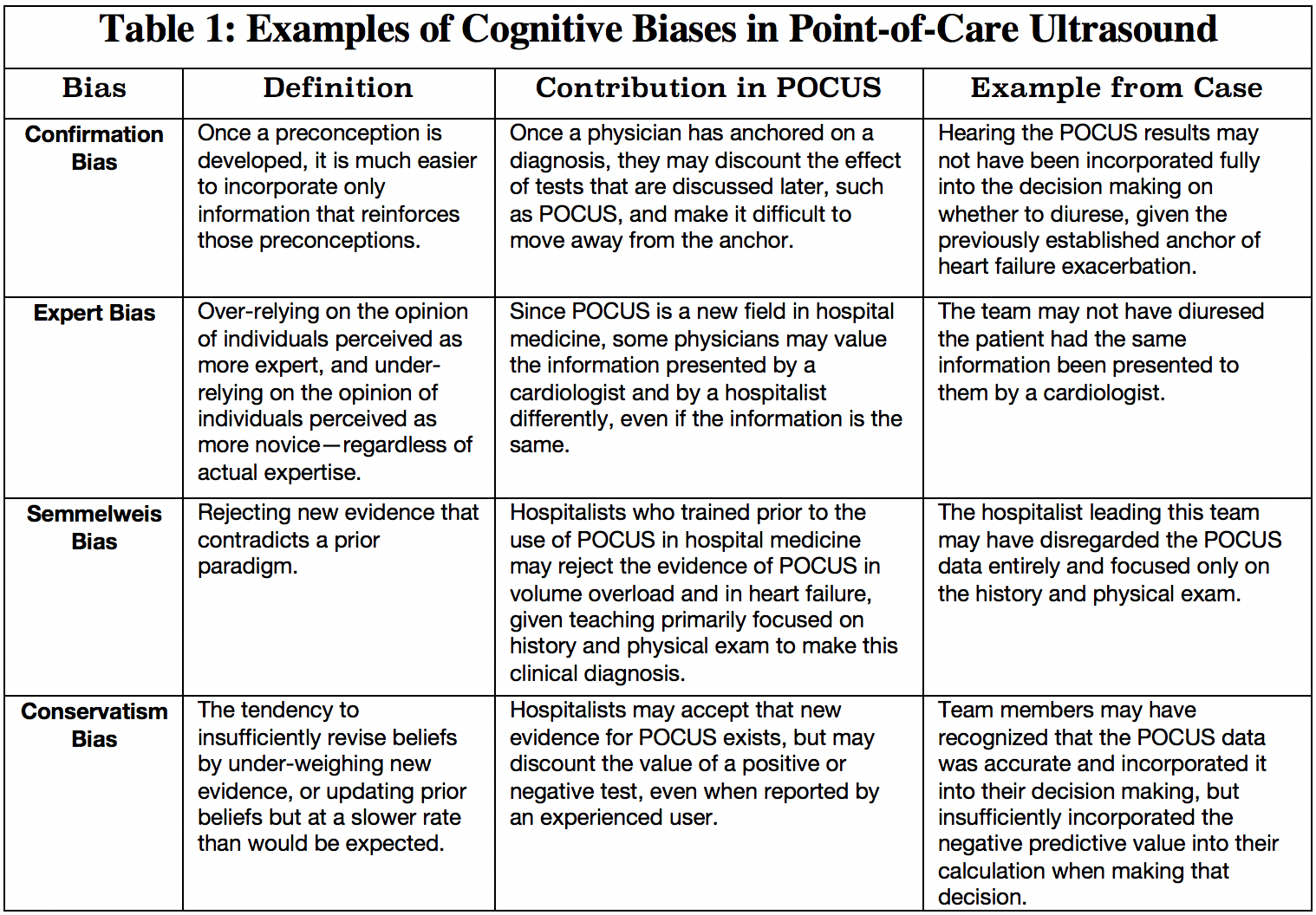
Discussion: Diagnostic error because of cognitive biases is thought to account for a substantial proportion of preventable errors in hospitalized patients, which can lead to avoidable patient harm. As POCUS is a relatively new diagnostic tool, clinicians may be prone to conservatism bias, Semmelweis bias, and others (table 1). Anchoring almost certainly played a role in this case as well—when it was presented that this woman had shortness of breath, a history of heart failure, and edema, the listening physician may have been biased that this patient has a heart failure exacerbation prior to hearing the POCUS exam. Additionally, clinicians may be unfamiliar with the positive and negative predictive value of POCUS exams and therefore unable to apply Bayesian reasoning. Inexperienced clinicians may lack confidence in their own POCUS exam and therefore underestimate the utility of POCUS generally.
Conclusions: Literature on POCUS has demonstrated a high negative predictive value for volume overload and heart failure exacerbation when used by a trained examiner in the correct clinical context. While POCUS literature and education often highlights the important limitations of POCUS, it is equally imperative to recognize the dangers of discounting a well-performed POCUS exam by an experienced user. POCUS credentialing and broader training of hospitalist may help mitigate the above biases and reduce diagnostic error.