Case Presentation:
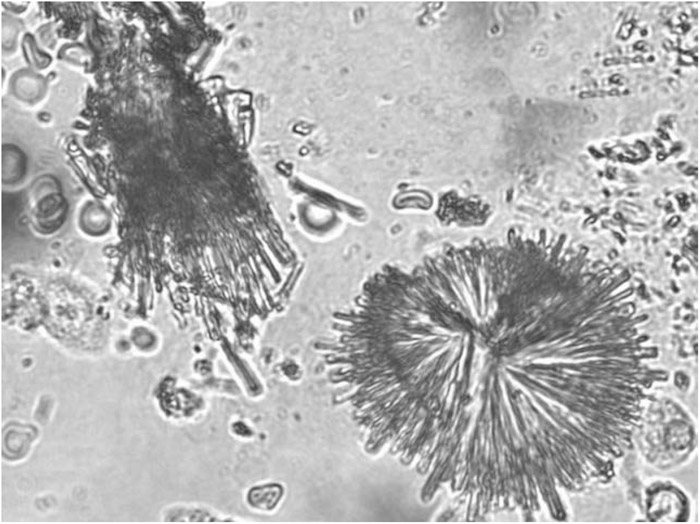
A 56‐year‐old man with recently diagnosed HIV‐associated toxoplasma encephalitis presented after a generalized seizure. Two weeks prior, he began treatment for toxoplasmosis with pyrimethamine, sulfadiazine, and leu‐covorin. His course was complicated by a presumed sulfadiazine‐induced drug rash and a readmission for seizure. Brain MRI showed improvement in brain lesions but laboratory studies revealed acute kidney injury (SCr, 0.8–1.6 mg/dL). Urinalysis reported hematuria, pyuria, and 4+ sodium urate crystals, suggesting acute urate nephropathy. Given the concern for sulfadiazine‐induced renal injury, we performed a lignin test, which was positive. Urine microscopy demonstrated “shocks‐of‐wheat” crystals, characteristic of sulfonamide crystals. The presumptive diagnosis was a combined picture of sulfadiazine hypersensitivity–mediated acute tubulointerstitial nephritis (AIN) and crystal nephropathy. Seizure was attributed to underlying brain lesions and pyrimethamine toxicity in the setting of renal failure.
Discussion:
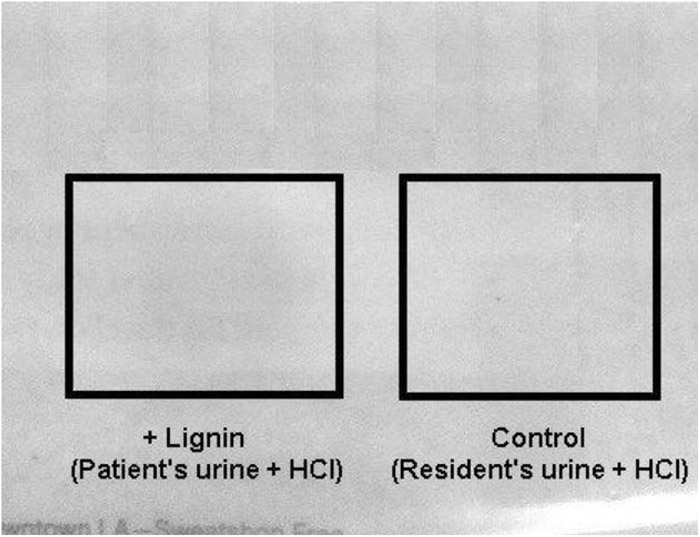
Hospitalists rely heavily on computer‐based reporting of clinical data, but analysis of primary data using simple tests remains useful. In this case, the initial urinalysis suggested acute urate nephropathy, although this diagnosis was inconsistent with the clinical picture. Uricemia was mild (8.5 mg/dL), and creatine kinase of 250 U/L argued against tissue catabolism from seizure as the cause. Given the suspicion for sulfadiazine crystalluria, we performed 2 simple tests: the lignin test and urine microscopy. The lignin test was performed by adding a drop of 10% HCl to a newspaper containing a drop of urine; a yellow‐orange color indicated sulfonamide crystals (Fig. 1). By microscopy, we then visualized amber, needle‐like crystals in “shocks of wheat” (Fig. 2). Urate crystals, in contrast, would have appeared as rhombic plates. Sulfonamides can cause renal failure by at least 2 mechanisms: hypersensitivity‐mediated AIN and tubular crystal precipitation. The former is unpredictable, whereas the latter is more commonly seen among immunocompromised patients receiving high‐dose sulfonamides. Both conditions may present with white and red cells in the urine sediment, although AIN does not typically present with crystalluria. In this unusual case, there was evidence of both processes.
Conclusions:
This case highlights the importance of primary data analysis in the context of the broader clinical picture. The case also raises awareness of sul‐fadiazine nephrotoxicity.
Disclosures:
D. Miller ‐ none; M. Fung ‐ none; G. Kim ‐ none