Case Presentation: A 26-year-old man with no significant past medical history presented to medical attention with severe oral mucositis. Approximately one week prior to his presentation, the patient developed symptoms of a respiratory illness with a productive cough, myalgias, and fever of up to 103 Fahrenheit. Although his respiratory symptoms began to improve, he developed severe mouth pain, eye redness and discharge, and pain with urination which prompted him to seek medical attention. He denied any new medications or changes in his medications. On physical exam, the patient was ill-appearing. He had severe oral mucositis with desquamating plaques throughout the oral mucosa with fissuring of the lips and yellow crust. His conjunctivae were injected with mucoid discharge from bilateral eyes. Erythematous vesicular lesions were noted on the scrotum and erythema was present at the urethral meatus. The patient was mildly tachycardic, with no appreciable murmurs and breath sounds had rales at the left lung base. Blood work was notable for undetectable HIV RNA, negative HSV/VZV, negative STI testing, and negative ANCA. Pneumonia PCR was positive for Mycoplasma pneumoniae. Chest CT showed tree-in-bud opacities in the left lower lobe suggestive of pneumonia. The patient was seen by the dermatology and ophthalmology services who felt the clinical presentation was consistent with diagnosis of Reactive Infectious Mucocutaneous Eruption (RIME) and he was started on treatment with IV methylprednisolone 1 mg/kg/day for 4 days with significant improvement followed by steroid taper. For his Mycoplasma infection, the patient was treated with a 3-day course of high-dose azithromycin.
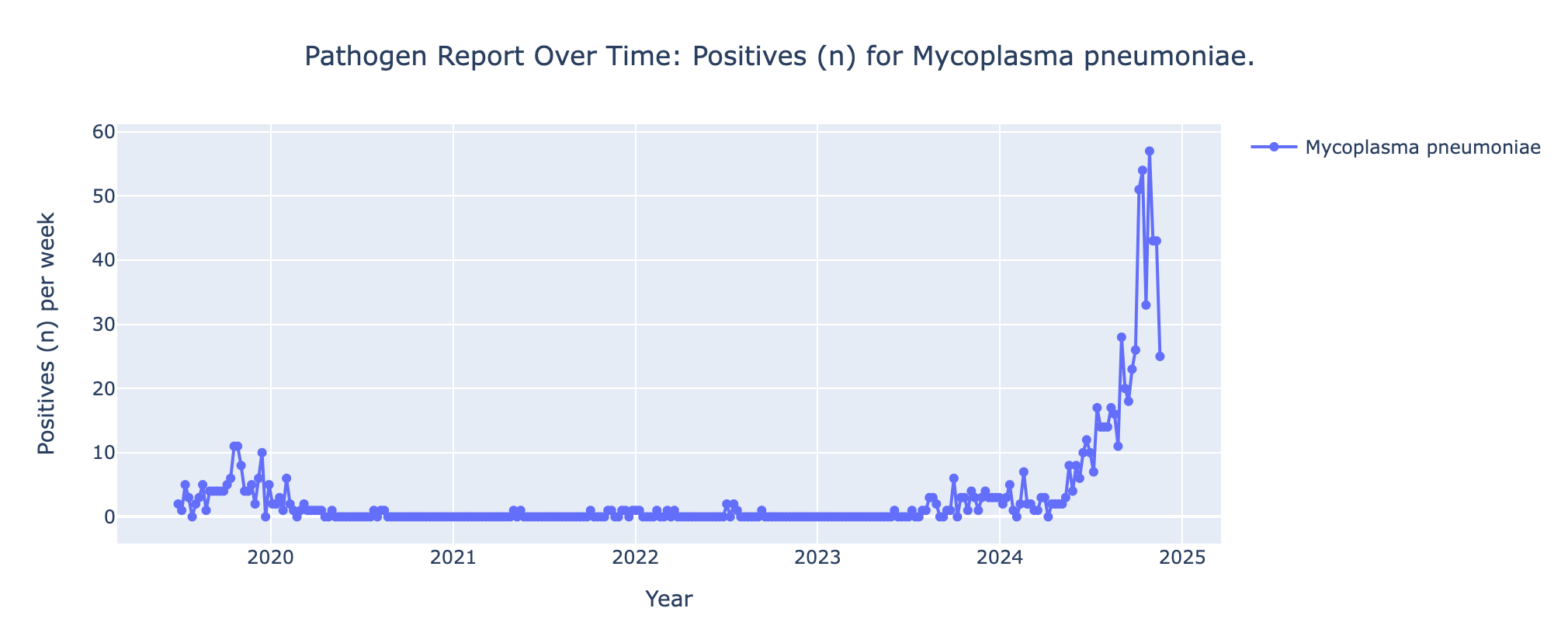
Discussion: Reactive Infectious Mucocutaneous Eruption (RIME) is characterized by severe mucositis triggered by bacterial or viral infections, most commonly Mycoplasma pneumoniae. Due to its strong association with Mycoplasma infections, the syndrome was previously called Mycoplasma pneumoniae-Induced Rash and Mucositis (MIRM) (1). However, the syndrome has since been observed following non-Mycoplasma infections including influenza B and coronaviruses prompting a change in terminology (2). The syndrome is most common in children, with a mean age of 11.9, however cases have also been reported in adults (3). In the United States, rates of Mycoplasma are the highest they have been in several recent years (4). Seasonal prevalence at our institution has been similarly high. Due to visual similarities with other dermatologic phenomena including Stevens-Johnson Syndrome (SJS)/toxic epidermal necrolysis (TEN) and erythema multiforme, RIME can to be misdiagnosed and is likely under-recognized. RIME should be considered in patients with a prodrome of viral respiratory symptoms followed by severe mucositis of two or more mucous membranes. Obtaining a RVP or sputum sample can be useful in identifying and treating inciting infections as in our case.
Conclusions: With the increasing incidence of Mycoplasma pneumoniae in the United States, it can be expected that the incidence of RIME will also increase. Thus, it will be important for clinicians to be aware of and have a strategy for management of this disease. RIME should be considered in patients presenting with oral, ocular, or urogenital mucosal ulcerations following a prodrome of upper respiratory symptoms. Our case demonstrates a successful approach to diagnosing and treating RIME in an adult patient with IV steroids followed by steroid taper in conjunction with symptomatic management.